The Role of Smart Wearables in Predicting Health Risks and Outcomes is exploding. Forget clunky medical equipment – tiny devices strapped to your wrist are now quietly collecting data that could revolutionize how we understand and prevent disease. From your heartbeat’s rhythm to your sleep patterns, these digital health companions offer a glimpse into your inner workings, potentially flagging serious health issues long before traditional methods. But is this a health revolution or just a tech trend? Let’s dive in.
This exploration delves into how smart wearables are transforming healthcare, analyzing their ability to predict cardiovascular disease, diabetes, respiratory problems, and even mental health challenges. We’ll examine the accuracy of this data, compare it to traditional methods, and discuss the ethical considerations surrounding such intimate health tracking. Get ready to uncover the potential – and the pitfalls – of this exciting technology.
Introduction to Smart Wearables and Health Data: The Role Of Smart Wearables In Predicting Health Risks And Outcomes
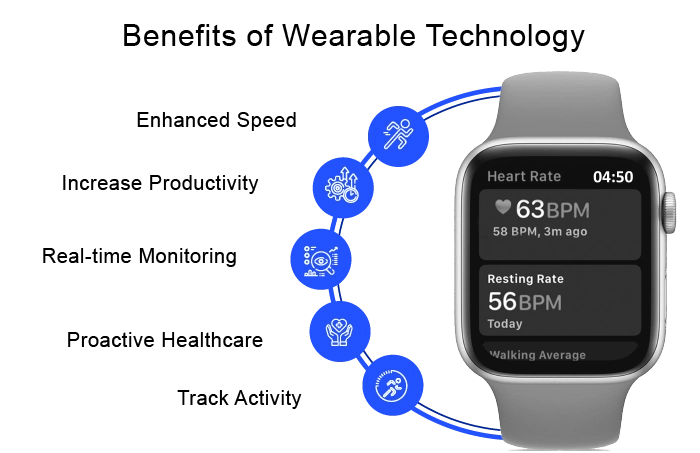
The rise of smart wearables has revolutionized personal health monitoring, transitioning from simple fitness trackers to sophisticated devices capable of collecting a wealth of physiological data. This miniaturization of powerful sensors has empowered individuals to take a more proactive role in managing their health, providing data that can be leveraged for early disease detection and personalized interventions. This evolution opens exciting possibilities for predictive healthcare, but also presents challenges in data interpretation and ethical considerations.
Smart wearables are essentially miniaturized medical-grade sensors worn on the body, continuously monitoring various physiological parameters. This constant stream of data offers a more comprehensive picture of an individual’s health than traditional periodic check-ups. This shift from episodic to continuous monitoring is a key driver of the potential for early disease detection and improved health outcomes.
Types of Physiological Data Collected by Smart Wearables
Various smart wearable devices collect a range of physiological data, offering a holistic view of an individual’s health status. This data is crucial for building predictive models and identifying potential health risks. The accuracy and reliability of this data vary depending on the device and its sensors.
- Heart Rate and Heart Rate Variability (HRV): Many wearables monitor heart rate continuously, providing insights into cardiovascular health. HRV, the variation in time between heartbeats, is a particularly valuable indicator of autonomic nervous system function and can signal potential stress or health issues. For example, consistently low HRV might suggest increased risk of cardiovascular events.
- Sleep Patterns: Wearables track sleep duration, sleep stages (light, deep, REM), and sleep quality. Disrupted sleep patterns are linked to various health problems, including obesity, cardiovascular disease, and mental health issues. Consistent monitoring allows for the identification of sleep disorders and the development of personalized sleep hygiene strategies.
- Activity Levels: Step counts, distance traveled, calories burned, and other activity metrics are commonly tracked. This data is crucial for assessing physical activity levels and identifying sedentary behavior, both of which are significant risk factors for various chronic diseases. For instance, consistently low activity levels could indicate a higher risk of developing type 2 diabetes.
- Electrocardiogram (ECG): Some advanced smartwatches incorporate ECG sensors, enabling the detection of irregular heart rhythms like atrial fibrillation. Early detection of atrial fibrillation is crucial, as it can significantly reduce the risk of stroke. Apple Watch, for example, has been shown to successfully detect atrial fibrillation in numerous users.
- Blood Oxygen Saturation (SpO2): This metric measures the percentage of hemoglobin in the blood that is saturated with oxygen. Low SpO2 levels can indicate respiratory problems, and continuous monitoring can provide early warnings of conditions like sleep apnea or COVID-19 complications. This data is particularly valuable for individuals with respiratory conditions.
Potential Benefits and Limitations of Using Smart Wearables for Health Risk Prediction
The use of smart wearables for health risk prediction offers numerous benefits, but it’s crucial to acknowledge the limitations. The technology’s potential to improve preventative care is substantial, but responsible implementation and data interpretation are paramount.
The potential benefits include early detection of health issues, personalized interventions, improved patient engagement, and reduced healthcare costs through preventative care. For example, early detection of atrial fibrillation through a smartwatch could prevent a potentially life-threatening stroke.
However, limitations exist. Data accuracy can vary across devices and individuals. Algorithms used for risk prediction may not be universally applicable, requiring further refinement and validation across diverse populations. Furthermore, data privacy and security are major concerns, requiring robust safeguards to protect sensitive health information. Finally, over-reliance on wearable data without proper medical consultation can lead to misinterpretations and potentially harmful self-diagnosis.
Predicting Cardiovascular Disease Risk
Smart wearables are rapidly transforming how we approach preventative healthcare, offering a potential game-changer in the fight against cardiovascular disease (CVD). By continuously monitoring vital signs, these devices provide a wealth of data that can be analyzed to identify individuals at high risk of developing CVD, paving the way for timely interventions and improved outcomes. This move towards proactive healthcare represents a significant shift from traditional reactive models.
The ability of smart wearables to detect early warning signs of CVD is particularly exciting. Traditional methods often rely on infrequent check-ups and may miss crucial indicators. Wearables, however, offer continuous monitoring, potentially catching subtle changes that might otherwise go unnoticed.
Smart wearables are revolutionizing preventative healthcare by collecting massive amounts of personal health data. But analyzing this data deluge for meaningful insights requires serious computational muscle, which is where the game-changer comes in: understanding how quantum computing will shape the future of data analysis, as explored in this insightful article How Quantum Computing Will Shape the Future of Data Analysis , is key to unlocking the full potential of wearable tech in predicting and preventing health risks.
This means more accurate, timely interventions, leading to healthier lives.
Early Warning Sign Detection with Smart Wearables
Smart wearables equipped with various sensors can detect several early warning signs of cardiovascular disease. For instance, irregularities in heart rhythm, such as atrial fibrillation (AFib), can be detected through electrocardiogram (ECG) sensors integrated into some smartwatches. Similarly, elevated heart rate variability (HRV), a measure of the variation in time between heartbeats, can indicate underlying cardiovascular issues. Consistent monitoring of heart rate and blood oxygen saturation (SpO2) can also reveal patterns suggestive of increased risk. The continuous nature of this data collection allows for the identification of trends that might be missed in sporadic clinical assessments.
Accuracy of Smart Wearable Data Compared to Traditional Methods
While smart wearables offer a promising avenue for CVD risk assessment, it’s crucial to acknowledge that their accuracy is not yet on par with traditional methods in all cases. Traditional methods, such as electrocardiograms (ECGs) performed in a clinical setting, echocardiograms, and blood tests, are generally considered the gold standard for diagnosing cardiovascular conditions. However, the continuous monitoring offered by wearables allows for the detection of subtle changes over time, providing a more comprehensive picture of an individual’s cardiovascular health. The data from wearables can supplement, rather than replace, traditional methods, leading to a more holistic and potentially more accurate assessment of risk. For example, a wearable might detect an irregular heartbeat pattern, prompting a referral for a more definitive ECG to confirm the diagnosis of AFib.
Machine Learning and Cardiovascular Event Prediction
The vast amounts of data generated by smart wearables are ideally suited for analysis using machine learning (ML) algorithms. ML algorithms can identify complex patterns and correlations in the data that might be missed by human observation. By training these algorithms on large datasets of wearable data combined with clinical outcomes, researchers are developing models that can predict the likelihood of future cardiovascular events with increasing accuracy. These models can incorporate various factors, such as age, sex, medical history, and lifestyle choices, along with the continuous physiological data from wearables, to provide a personalized risk assessment. For instance, a model might identify individuals at high risk of a heart attack based on patterns in their heart rate, sleep patterns, and activity levels detected by their wearable device. This allows for timely interventions, such as lifestyle modifications or medication adjustments, to mitigate the risk.
Comparison of Smart Wearable Sensors for Cardiovascular Risk Prediction
| Device | Sensor Type | Data Accuracy | Limitations |
|---|---|---|---|
| Apple Watch (with ECG) | ECG, Heart Rate, Accelerometer | High accuracy for detecting AFib; moderate accuracy for heart rate variability | Accuracy can be affected by factors like skin contact and user movement; not suitable for all individuals. |
| Fitbit Sense | ECG, Heart Rate, SpO2, EDA | Moderate accuracy for detecting AFib and heart rate variability; SpO2 accuracy varies. | Requires proper calibration and consistent wear; may not detect all types of heart rhythm abnormalities. |
| Garmin Venu 2 Plus | Heart Rate, SpO2, Accelerometer | Moderate accuracy for heart rate and SpO2; limited ability to detect arrhythmias. | Data accuracy depends on individual factors and proper device use; lacks ECG functionality. |
| Samsung Galaxy Watch 4 | ECG, Heart Rate, SpO2 | High accuracy for detecting AFib; moderate accuracy for heart rate variability | May not be suitable for all individuals; data accuracy can be affected by various factors. |
Assessing and Predicting Diabetes Risk

Source: xevensolutions.com
Smart wearables are quietly revolutionizing preventative healthcare, and their potential in predicting and managing diabetes is particularly exciting. By passively monitoring various physiological parameters, these devices offer a window into an individual’s metabolic health, potentially identifying those at risk long before traditional diagnostic methods. This allows for early intervention and personalized prevention strategies, ultimately improving outcomes and reducing the burden of this chronic disease.
Smart wearables contribute to diabetes risk assessment by tracking key physiological indicators closely linked to glucose metabolism and overall health. This data, collected continuously and non-invasively, offers a far richer picture than sporadic clinical measurements. The continuous monitoring allows for the identification of subtle changes that might otherwise go unnoticed, paving the way for proactive interventions.
Key Physiological Parameters and Diabetes Risk
Several physiological parameters tracked by smart wearables are directly relevant to assessing diabetes risk. These parameters, when analyzed together, provide a holistic view of an individual’s metabolic health and can help identify patterns indicative of developing diabetes. Crucially, these parameters are often collected passively, making the process convenient and less intrusive than traditional methods.
Blood glucose levels, while not directly measured by most consumer wearables, can be indirectly inferred through analysis of other parameters like sleep patterns, activity levels, and heart rate variability. Activity levels, particularly the consistency and intensity of physical activity, are strongly correlated with glucose control. Poor sleep quality is also associated with increased risk of insulin resistance and type 2 diabetes. Heart rate variability (HRV), a measure of the variation in time between heartbeats, reflects the balance of the autonomic nervous system and can indicate stress levels, which are known to impact glucose metabolism.
Studies Utilizing Smart Wearable Data for Diabetes Prediction
Several studies have demonstrated the potential of smart wearable data in predicting diabetes onset or progression. For example, a study published in the journal *Diabetes Care* analyzed data from smartwatches to identify patterns in activity levels, sleep duration, and heart rate variability that were predictive of developing type 2 diabetes. The researchers found that individuals exhibiting specific patterns of these parameters had a significantly higher risk of developing the condition within the next few years. Another study, using data from continuous glucose monitors (CGMs) integrated with smartwatches, showed promising results in identifying early signs of insulin resistance, a precursor to type 2 diabetes. These studies highlight the power of combining multiple data streams from smart wearables to create a more comprehensive and accurate risk assessment.
Personalizing Diabetes Prevention Strategies with Smart Wearable Data
Imagine Sarah, a 35-year-old woman with a family history of type 2 diabetes. Her smartwatch, consistently tracking her activity levels, sleep quality, and resting heart rate, reveals a pattern of low activity, poor sleep, and elevated resting heart rate. This data, combined with her family history, suggests a heightened risk of developing diabetes. Based on this information, a personalized intervention plan could be developed. This might include recommendations for increasing physical activity, improving sleep hygiene, and managing stress levels – all tailored to Sarah’s specific lifestyle and preferences. Regular feedback from the smartwatch, showing progress towards her goals, can reinforce positive behavioral changes and help her stay motivated. This proactive, personalized approach, driven by the data collected by smart wearables, significantly improves the chances of preventing the onset of diabetes.
Monitoring and Predicting Respiratory Health Issues
Source: delveinsight.com
Smart wearables are increasingly proving their worth beyond fitness tracking. Their ability to continuously monitor physiological data opens exciting possibilities for early detection and management of respiratory conditions, potentially revolutionizing healthcare. By leveraging miniaturized sensors and sophisticated algorithms, these devices offer a convenient and accessible way to monitor respiratory health, paving the way for proactive interventions.
Smart wearables can passively monitor several key respiratory parameters, providing valuable insights into an individual’s respiratory health. This continuous monitoring allows for the identification of subtle changes that might otherwise go unnoticed, enabling timely intervention and potentially preventing serious complications.
Respiratory Rate Monitoring and Analysis
Smartwatches and fitness trackers often incorporate optical sensors that measure heart rate. These same sensors, along with accelerometers, can indirectly estimate respiratory rate by detecting subtle chest movements associated with breathing. Algorithms analyze the variations in these signals to identify patterns indicative of abnormal breathing rates, such as tachypnea (rapid breathing) or bradypnea (slow breathing), both of which can be symptoms of underlying respiratory issues. For instance, a consistent elevation in respiratory rate beyond a healthy range, coupled with other data points, might trigger an alert suggesting the need for medical attention. The accuracy of these estimations varies depending on the device and the algorithm used, but improvements are constantly being made. More sophisticated devices might incorporate dedicated respiratory sensors for increased precision.
Sleep Apnea Detection
Sleep apnea, a condition characterized by pauses in breathing during sleep, is often diagnosed through polysomnography, a complex and expensive sleep study. However, smart wearables, equipped with accelerometers and oximeters (measuring blood oxygen saturation), can contribute to the detection of sleep apnea. These devices monitor movement and oxygen levels throughout the night. Frequent drops in oxygen saturation or disrupted sleep patterns detected by the accelerometer can suggest potential sleep apnea. While wearables cannot provide a definitive diagnosis, they can flag individuals at high risk, prompting them to seek professional medical evaluation. Algorithms analyzing this data look for patterns such as prolonged periods of low oxygen levels or frequent awakenings during sleep, typical indicators of apnea events.
Comparison of Smart Wearables for Respiratory Health Monitoring
The market offers a variety of smart wearables designed for respiratory health monitoring, each with its strengths and weaknesses. Choosing the right device depends on individual needs and budget.
Here’s a comparison of some key factors:
- Accuracy: Accuracy varies significantly between devices. Some rely on indirect measurements (e.g., using heart rate variability to infer respiratory rate), leading to lower accuracy than dedicated respiratory sensors. Devices using dedicated sensors generally provide more accurate data, but may be more expensive.
- Cost: Prices range widely, from relatively inexpensive fitness trackers to more costly medical-grade devices with advanced features and higher accuracy. The cost often correlates with the level of sophistication and accuracy of the sensors and algorithms used.
- User-Friendliness: Some devices are easier to use and interpret than others. Factors such as the app interface, data presentation, and ease of setup influence user experience. Intuitive interfaces and clear data visualization are essential for user adoption and adherence to monitoring protocols.
Mental Health Monitoring and Risk Prediction
Smart wearables are increasingly recognized for their potential beyond physical health tracking. Their ability to passively collect physiological data offers a unique window into mental well-being, paving the way for earlier detection and intervention in mental health conditions. This capability stems from the correlation between physiological signals and mental states, enabling the identification of patterns indicative of mental health risks.
The continuous monitoring capabilities of smart wearables allow for the capture of subtle changes in physiological parameters, offering a more comprehensive picture of an individual’s mental health compared to traditional methods reliant on infrequent clinical visits or self-reporting. This continuous data stream holds immense promise for early risk detection and personalized interventions.
Sleep Patterns as Indicators of Mental Health
Sleep disturbances are frequently associated with various mental health conditions, including anxiety and depression. Smartwatches and fitness trackers equipped with sleep-tracking features can objectively quantify sleep duration, sleep stages (light, deep, REM), and sleep fragmentation. For example, consistently reduced total sleep time, increased wakefulness after sleep onset, or a significant decrease in deep sleep can be flagged as potential indicators warranting further investigation. These data points, when combined with other information, can contribute to a more comprehensive assessment of mental health risk. Analysis of sleep patterns over extended periods can also reveal trends and changes indicative of worsening mental health, prompting timely interventions.
Activity Levels and Mental Well-being
Physical activity is strongly linked to mental health. Smart wearables can accurately track daily steps, distance covered, and exercise duration. Consistent inactivity or a sudden significant drop in activity levels can be a warning sign, particularly when coupled with other indicators like changes in sleep patterns. For instance, a person experiencing a depressive episode might exhibit a marked reduction in their daily activity, providing valuable information for healthcare professionals. Conversely, increased activity can be a positive indicator of improved mental health. The objective measurement of activity levels provides a quantifiable metric for monitoring progress during treatment.
Heart Rate Variability (HRV) and Mental Stress
Heart rate variability, the variation in time intervals between heartbeats, is a sensitive indicator of autonomic nervous system activity. Smart wearables can readily measure HRV, and reduced HRV is often associated with increased stress and heightened risk of mental health issues. Studies have shown that individuals experiencing chronic stress or anxiety often exhibit lower HRV compared to their healthier counterparts. Monitoring HRV over time can provide valuable insights into an individual’s stress levels and potential mental health risks. For example, a consistent decline in HRV coupled with reported anxiety could prompt earlier intervention.
Integration of Wearable Data with Other Data Sources
The power of smart wearable data in mental health monitoring is amplified when integrated with other data sources. Combining physiological data from wearables with self-reported data from questionnaires or apps, and clinical data from medical records, can create a holistic picture of an individual’s mental health. This integrated approach can lead to more accurate risk prediction and personalized interventions. For example, a person reporting feelings of anxiety alongside consistently low HRV and disrupted sleep patterns would have a higher predicted risk than someone exhibiting only one of these indicators.
Ethical Considerations in Mental Health Monitoring
The use of smart wearable data for mental health monitoring raises several ethical considerations. Data privacy and security are paramount. Robust measures must be in place to protect sensitive personal data from unauthorized access and misuse. Informed consent is crucial; individuals must be fully aware of how their data will be collected, used, and shared. Transparency regarding algorithms and decision-making processes is also essential to build trust and ensure fairness. Furthermore, the potential for bias in algorithms and the risk of stigmatization need careful consideration. The responsible and ethical implementation of this technology requires a multi-faceted approach that prioritizes individual rights and well-being.
Challenges and Future Directions
The exciting potential of smart wearables in revolutionizing healthcare is undeniable, but several hurdles need to be overcome before widespread adoption and accurate prediction become reality. Navigating these challenges requires a multi-pronged approach involving technological advancements, ethical considerations, and robust regulatory frameworks.
Data accuracy, privacy, and interpretation present significant obstacles. The reliability of wearable sensor data can be impacted by factors like individual variations in physiology, device placement, and environmental interference. This necessitates the development of more sophisticated algorithms capable of filtering noise and accurately interpreting the data. Simultaneously, the sensitive nature of health data raises critical privacy concerns, demanding robust security measures and transparent data handling practices. Finally, the sheer volume and complexity of data generated require advanced analytical techniques to extract meaningful insights and translate them into actionable predictions.
Data Accuracy and Reliability
Improving the accuracy and reliability of smart wearable data is paramount. This involves not only refining the sensor technology itself but also developing more robust algorithms for data processing and analysis. For instance, algorithms could be designed to account for individual differences in skin tone affecting heart rate variability measurements from optical sensors, or compensate for movement artifacts that interfere with accurate step counting. Furthermore, integrating data from multiple wearables or cross-referencing with other health information could provide a more holistic and accurate picture. Consider the example of a smartwatch measuring heart rate alongside a smart scale tracking weight – combining this data could offer a more nuanced view of cardiovascular health than either source alone.
Data Privacy and Security, The Role of Smart Wearables in Predicting Health Risks and Outcomes
Protecting the privacy and security of health data collected by smart wearables is critical. This requires robust encryption protocols, secure data storage solutions, and transparent data governance policies. Regulations like GDPR in Europe and HIPAA in the United States provide a framework, but continuous adaptation is needed to keep pace with evolving technologies and threats. Furthermore, empowering individuals with greater control over their data, allowing them to choose what is shared and with whom, is essential for building trust and encouraging adoption. A system where users can easily review and delete their data, and understand how it’s being used, is key.
Data Interpretation and Integration with Other Technologies
The sheer volume of data generated by smart wearables necessitates advanced analytical techniques to extract meaningful insights. Artificial intelligence (AI), particularly machine learning, plays a crucial role here. AI algorithms can identify patterns and correlations in large datasets that might be missed by human analysts, leading to more accurate and timely risk predictions. Moreover, integrating smart wearable data with electronic health records (EHRs), genomic information, and lifestyle data can provide a far more comprehensive view of an individual’s health status. Imagine a system where AI analyzes data from a smartwatch, a fitness tracker, and an EHR to predict the likelihood of a diabetic patient developing complications, allowing for proactive intervention.
Future Potential of Smart Wearables in Personalized Healthcare
Imagine a futuristic illustration: a vibrant, interactive dashboard displays a personalized health profile. It seamlessly integrates data from a variety of smart wearables—a smartwatch monitoring heart rate and sleep, a smart scale tracking weight and body composition, and a smart patch analyzing sweat for biomarkers. This data is dynamically analyzed by AI, providing real-time insights into the individual’s health status and predicting potential risks. The dashboard visually represents this information with clear, easy-to-understand graphs and charts, offering personalized recommendations for lifestyle changes, medication adjustments, or medical consultations. The overall tone is one of empowerment, placing the individual firmly in control of their health journey, guided by data-driven insights and personalized support. This system actively learns and adapts to the individual’s unique needs, evolving into a truly personalized healthcare companion.
Final Conclusion

Source: themindstudios.com
Smart wearables aren’t a magic bullet, but they represent a powerful shift in preventative healthcare. While challenges remain in data accuracy, privacy, and interpretation, the potential for personalized health monitoring and early disease detection is undeniable. As technology continues to advance, the integration of AI and big data analytics will only enhance the predictive power of these tiny devices, paving the way for a future where proactive healthcare is the norm, not the exception. The future of health is on your wrist.
