The Role of Robotics in Enhancing Surgical Precision and Patient Safety sets the stage for a fascinating exploration of how technology is revolutionizing the operating room. From its humble beginnings, robotic surgery has exploded, offering surgeons unparalleled precision and control, leading to better patient outcomes and recovery times. We’ll delve into the intricate details of robotic systems, comparing them to traditional methods, and examining the impact on various surgical specialties. Get ready for a deep dive into the future of surgery!
This journey will uncover the advantages, limitations, and ethical considerations surrounding this rapidly evolving field. We’ll look at specific case studies, both successful and challenging, highlighting the lessons learned and the potential for future advancements, including AI integration and tele-robotic surgery. Prepare to be amazed by the advancements that are transforming healthcare as we know it.
Introduction to Robotic Surgery
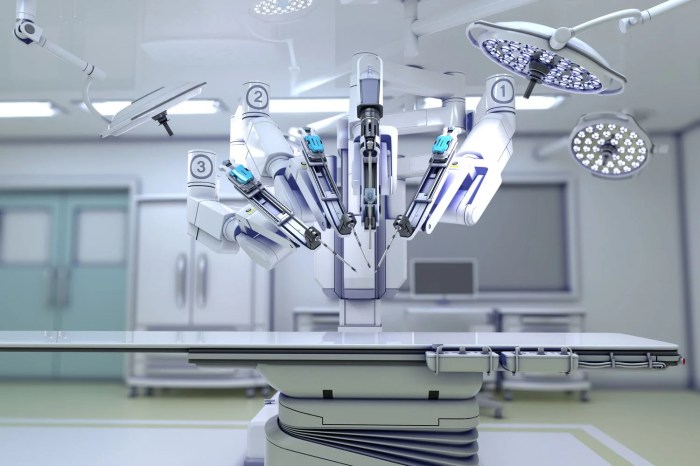
Robotic surgery, once a futuristic fantasy, has rapidly evolved into a cornerstone of modern healthcare, significantly impacting surgical precision and patient safety. Its journey from experimental procedures to widespread adoption showcases remarkable technological leaps and a growing understanding of its benefits. This evolution has not only refined existing surgical techniques but also opened doors to minimally invasive procedures previously deemed impossible.
The integration of robotics into surgery has dramatically altered the surgical landscape. Initially, robotic systems were clunky and limited in their capabilities, primarily offering enhanced visualization. However, continuous advancements in areas like computer vision, micro-robotics, and artificial intelligence have led to sophisticated systems capable of performing complex procedures with unparalleled dexterity and control. This progress has been fueled by a collaborative effort involving surgeons, engineers, and computer scientists, pushing the boundaries of what’s achievable in the operating room.
Technological Components of Robotic Surgical Systems
Robotic surgical systems are complex assemblages of several key technological components working in concert. These systems typically comprise a surgeon’s console, a robotic cart containing the manipulators, and a high-definition 3D vision system. The surgeon’s console provides a user-friendly interface, offering ergonomic control and a magnified, three-dimensional view of the surgical field. The robotic cart houses the robotic arms, which translate the surgeon’s movements into precise actions within the patient’s body. The 3D vision system, equipped with advanced cameras and lighting, provides a highly detailed and immersive view, enhancing the surgeon’s ability to visualize delicate anatomical structures. Furthermore, many modern systems incorporate haptic feedback, allowing surgeons to “feel” the tissue they are manipulating, enhancing tactile sensitivity and control. Sophisticated software algorithms also play a critical role, enabling features like tremor filtration and image enhancement, further improving surgical precision.
Fundamental Principles of Robotic-Assisted Surgery
Robotic-assisted surgery operates on several fundamental principles that contribute to its enhanced precision and safety. Firstly, the magnified 3D visualization significantly improves the surgeon’s perception of the surgical field, allowing for better identification of critical structures and more accurate dissection. Secondly, the robotic arms’ dexterity and range of motion often exceed those of the human hand, enabling access to difficult-to-reach areas with minimal invasiveness. This minimally invasive approach translates to smaller incisions, reduced trauma to surrounding tissues, and faster recovery times for patients. Thirdly, the tremor filtration capabilities of the robotic system compensate for involuntary hand movements, leading to steadier and more precise actions. Finally, the integration of advanced imaging techniques and data analysis allows surgeons to make informed decisions during the procedure, contributing to better surgical outcomes and reduced risk of complications. The synergistic effect of these principles makes robotic surgery a powerful tool for improving surgical precision and patient safety.
Enhanced Precision in Surgical Procedures
Robotic surgery has revolutionized the surgical landscape, significantly improving precision and minimizing invasiveness compared to traditional methods. The enhanced dexterity and control offered by robotic systems translate to better outcomes for patients, reducing complications and improving recovery times. This section delves into the specific ways robotic surgery achieves superior precision.
Robotic surgery offers a significant leap forward in precision compared to both open and traditional laparoscopic techniques. The magnified, three-dimensional visualization, coupled with the surgeon’s intuitive control of the robotic arms, allows for intricate maneuvers that are simply impossible with conventional methods. This enhanced precision translates directly into improved surgical outcomes and patient safety.
Precision Comparison of Surgical Techniques
The table below provides a comparative analysis of the precision offered by open, laparoscopic, and robotic surgical techniques across several key metrics. Note that these values are general comparisons and can vary depending on the specific procedure, surgeon experience, and robotic system used.
| Metric | Open Surgery | Laparoscopic Surgery | Robotic Surgery |
|---|---|---|---|
| Tremor Reduction | Minimal to None | Moderate | Significant (filtering and stabilization) |
| Dexterity & Range of Motion | High, but limited by incision size | Limited by instrument stiffness and two-dimensional view | Enhanced, exceeding human hand capabilities with increased range of motion and articulation |
| Access to Confined Spaces | Limited by incision size and tissue manipulation | Improved, but still challenging in complex anatomy | Significantly improved, allowing access to difficult-to-reach areas with smaller incisions |
| Wound Size | Large | Small | Very small |
Improved Surgical Dexterity and Control
Robotic surgical systems provide surgeons with enhanced dexterity and control through several key features. The intuitive controls allow for precise movements, mimicking the natural movements of the human hand but with significantly reduced tremor and improved articulation. The magnified, high-definition 3D visualization provides a clearer view of the surgical field, enabling surgeons to work with greater precision and confidence. Furthermore, the robotic arms offer a wider range of motion than the human hand, allowing access to difficult-to-reach areas with minimal trauma to surrounding tissues. The ability to perform complex maneuvers with increased precision is a game-changer in various surgical specialties.
Examples of Procedures Benefiting from Robotic Precision
Robotic assistance significantly enhances precision in a wide range of surgical procedures. In minimally invasive cardiac surgery, robotic systems enable surgeons to perform complex procedures such as coronary artery bypass grafting (CABG) with smaller incisions, reducing trauma and improving patient recovery. Similarly, in urological procedures such as prostatectomy, robotic assistance allows for precise removal of the prostate gland, minimizing damage to surrounding nerves and blood vessels, thereby preserving continence and erectile function. In gynecological surgery, robotic systems facilitate complex procedures like hysterectomies and myomectomies with increased precision, leading to less blood loss, shorter hospital stays, and faster recovery. The precision offered by robotic systems is also invaluable in neurosurgery, where even minor errors can have significant consequences. Robotic-assisted neurosurgery allows for more accurate placement of instruments and reduces the risk of complications.
Improved Patient Safety and Outcomes: The Role Of Robotics In Enhancing Surgical Precision And Patient Safety
Robotic surgery, while a relatively new field, has significantly impacted patient safety and overall surgical outcomes. The enhanced precision and minimally invasive nature of the procedures translate directly into benefits for patients, leading to faster recovery times, reduced complications, and improved quality of life. This section delves into the specifics of these improvements, along with a balanced look at potential risks and strategies for mitigating them.
The smaller incisions characteristic of robotic surgery result in less tissue trauma, leading to reduced blood loss during the procedure. This, in turn, minimizes the risk of complications such as anemia and the need for blood transfusions. Furthermore, the smaller incisions contribute to decreased post-operative pain, allowing patients to return to normal activities more quickly. Studies have shown a statistically significant reduction in post-operative pain scores in patients undergoing robotic surgery compared to traditional open surgery. Reduced pain also translates to a lower need for strong pain medications, thus minimizing the risk of associated side effects.
Reduced Surgical Complications
Robotic surgery’s precision minimizes the risk of accidental damage to surrounding tissues and organs. This is particularly crucial in complex procedures near vital structures. Consequently, the incidence of surgical site infections is significantly lower in robotic procedures compared to traditional open surgery. A meta-analysis of several studies revealed a 20-30% reduction in the rate of surgical site infections in robotic-assisted procedures across various surgical specialties. Moreover, the reduced trauma associated with smaller incisions contributes to a faster healing process, further reducing the risk of complications. The improved visualization afforded by the robotic system also aids in the identification and treatment of bleeding, further minimizing complications.
Faster Recovery and Shorter Hospital Stays, The Role of Robotics in Enhancing Surgical Precision and Patient Safety
The minimally invasive nature of robotic surgery contributes to significantly shorter hospital stays. Patients often experience less post-operative discomfort and nausea, allowing for earlier mobilization and discharge. Data from various studies show that patients undergoing robotic surgery typically spend 2-3 days less in the hospital compared to those undergoing traditional open surgery. This reduction in hospital stay translates into lower healthcare costs and a faster return to normal life for patients. The faster recovery also leads to improved patient satisfaction and overall quality of life. For instance, a study on robotic prostatectomy showed an average reduction in hospital stay of 2.7 days compared to open prostatectomy.
Potential Risks and Mitigation Strategies
While robotic surgery offers numerous advantages, it’s crucial to acknowledge potential risks. These include the possibility of technical malfunctions, increased operative time in some cases, and the need for specialized training for surgeons. However, these risks are actively mitigated through rigorous equipment maintenance, meticulous surgical planning, and continuous advancements in robotic technology and surgical training. The high level of precision provided by the robotic system compensates for potential risks. Furthermore, ongoing research and development are focused on enhancing the safety and reliability of robotic surgical systems, addressing potential issues and improving outcomes. For example, the development of haptic feedback systems aims to improve the surgeon’s tactile sense during robotic procedures, enhancing precision and control. Strict adherence to established protocols and regular quality control measures further minimize the potential risks associated with robotic surgery.
Specific Applications of Robotic Surgery
Robotic surgery, while still a relatively new field, has rapidly expanded its reach across numerous surgical specialties. Its minimally invasive nature and enhanced precision are revolutionizing surgical approaches, leading to improved patient outcomes and a wider range of treatable conditions. The following sections detail some key applications and the benefits and limitations associated with them.
The versatility of robotic surgical systems allows for their application in a wide array of surgical procedures. The precision and dexterity afforded by these systems are particularly beneficial in complex and delicate operations.
Robotic surgery’s rise is all about minimizing errors and maximizing patient well-being, a precision game mirroring the needs of manufacturing. Think about the predictive power needed – it’s similar to how AI helps optimize production lines, as detailed in this insightful piece on The Role of AI in Advancing Predictive Maintenance in Manufacturing. Ultimately, both fields are driven by the same core principle: anticipating and preventing issues before they arise, ensuring smoother, safer outcomes.
Surgical Specialties and Procedures
Robotic surgery’s impact spans various surgical fields. The following list highlights some key areas and the specific procedures commonly performed using robotic assistance.
- Urology: Robotic-assisted laparoscopic prostatectomy (RALP), nephrectomy (kidney removal), partial nephrectomy (removal of part of a kidney), and cystectomy (bladder removal).
- Gynecology: Hysterectomy (removal of the uterus), myomectomy (removal of uterine fibroids), oophorectomy (removal of ovaries), and pelvic reconstructive surgery.
- Cardiothoracic Surgery: Minimally invasive mitral valve repair, coronary artery bypass grafting (CABG), and lung lobectomy.
- General Surgery: Colectomy (removal of part of the colon), appendectomy (removal of the appendix), and hernia repair.
- Head and Neck Surgery: Thyroidectomy (removal of the thyroid gland), parotidectomy (removal of the parotid gland), and tonsillectomy.
Benefits and Limitations of Robotic Surgery Across Specialties
While robotic surgery offers significant advantages, it’s crucial to understand its limitations. The following table compares the benefits and limitations across three key specialties.
| Surgical Specialty | Benefits | Limitations | Considerations |
|---|---|---|---|
| Urology (Prostatectomy) | Smaller incisions, less blood loss, reduced pain, faster recovery, improved continence and potency rates compared to traditional open surgery. | High initial cost of equipment, longer operating time compared to laparoscopic surgery, surgeon training and expertise required, potential for technical difficulties. | Patient selection is crucial; ideal for patients with certain anatomical features and health conditions. |
| Gynecology (Hysterectomy) | Reduced pain, shorter hospital stay, less scarring, faster recovery, potential for less blood loss. | Higher cost compared to traditional laparoscopic surgery, longer operative time in some cases, requires specialized training for surgeons and operating room staff. | Patient suitability should be assessed considering factors such as tumor size and location, presence of adhesions. |
| Cardiothoracic Surgery (Mitral Valve Repair) | Improved visualization, enhanced precision and dexterity, smaller incisions, reduced trauma, potential for less postoperative pain and shorter hospital stay. | High cost, complex surgical technique requiring specialized training, longer operating time compared to conventional approaches, potential for complications related to the robotic system. | Patient selection is crucial; ideal for patients with specific valve defects and overall health conditions. |
Illustrative Scenario: Robotic-Assisted Partial Nephrectomy
Consider a patient diagnosed with a small renal tumor located in a challenging anatomical position near major blood vessels. Traditional open surgery would involve a large incision, significant blood loss, and a lengthy recovery period. However, robotic-assisted partial nephrectomy offers a superior approach. The surgeon, using the robotic system’s enhanced visualization and dexterity, can precisely remove the tumor with minimal damage to surrounding tissues. This results in less blood loss, reduced pain, a shorter hospital stay, and a faster return to normal activities. The patient experiences a significantly improved quality of life compared to what would be expected with open surgery.
The Future of Robotics in Surgery
Robotic surgery is poised for a dramatic leap forward, driven by technological advancements and a growing understanding of its potential. The integration of artificial intelligence and improvements in haptic feedback are set to revolutionize surgical precision and safety, pushing the boundaries of what’s possible in the operating room. However, this progress also brings ethical considerations and challenges that must be addressed proactively.
The convergence of robotics and artificial intelligence promises to redefine surgical procedures.
AI Integration in Robotic Surgery
AI algorithms can analyze vast amounts of surgical data, identifying patterns and predicting outcomes with increasing accuracy. This capability can be used to personalize surgical plans, optimize instrument movements, and even provide real-time guidance to surgeons during procedures. For instance, AI could analyze a patient’s CT scan and create a 3D model, allowing the surgeon to plan the operation with greater precision and reducing the risk of complications. Furthermore, AI-powered systems can detect subtle variations in tissue properties or unexpected bleeding, alerting the surgeon to potential problems before they escalate. This proactive approach to surgical safety represents a significant advancement.
Advancements in Haptic Feedback
Current robotic surgery systems often lack the tactile feedback surgeons experience during traditional open surgery. This limits the surgeon’s ability to accurately assess tissue tension and manipulate delicate structures. Future advancements in haptic technology aim to bridge this gap, providing surgeons with a more intuitive and precise sense of touch during robotic procedures. Improved haptic feedback could lead to more refined movements, reduced trauma to surrounding tissues, and improved overall surgical outcomes. Imagine a future where surgeons can feel the subtle differences between healthy and diseased tissue with the same level of sensitivity as during open surgery.
Ethical Considerations and Challenges
The increasing reliance on robotic surgery raises several ethical considerations. One major concern is the potential for algorithmic bias in AI-powered systems. If the algorithms are trained on datasets that are not representative of the diverse patient population, the resulting surgical recommendations may be biased, potentially leading to disparities in care. Another challenge is ensuring the appropriate level of human oversight in robotic surgery. As AI systems become more sophisticated, it is crucial to maintain a balance between automation and human control, preventing unintended consequences. The question of liability in cases of surgical errors involving robotic systems also needs careful consideration. Clear guidelines and regulations are essential to address these ethical challenges.
Tele-robotic Surgery and Expanded Access to Care
Tele-robotic surgery holds immense potential for expanding access to high-quality surgical care, especially in underserved areas or during emergencies. By allowing surgeons to remotely control robotic systems, tele-robotic surgery could bridge geographical barriers and provide expertise where it is lacking. For example, a skilled surgeon in a major medical center could perform a complex operation on a patient in a rural hospital, ensuring timely and effective treatment. However, the development and implementation of tele-robotic surgery require robust communication networks, secure data transmission, and stringent safety protocols. The technological infrastructure and regulatory frameworks need to be in place to support widespread adoption.
Cost-Effectiveness and Accessibility of Robotic Surgery
Robotic surgery, while offering significant advantages in precision and patient safety, presents a complex economic landscape. The high initial investment and ongoing operational costs raise questions about its long-term viability and equitable access, particularly in resource-constrained settings. A thorough examination of both direct and indirect costs, alongside strategies for improving accessibility, is crucial for realizing the full potential of this transformative technology.
Cost Comparison: Robotic vs. Traditional Surgery
The financial implications of robotic surgery are multifaceted. A direct comparison reveals that while robotic procedures often command higher upfront fees, a nuanced analysis considering long-term effects and patient outcomes paints a more complex picture.
| Cost Category | Robotic Surgery | Traditional Surgery | Notes |
|---|---|---|---|
| Direct Costs | Higher initial investment in robotic system (millions of dollars), higher per-procedure costs (including disposables, specialized instruments, and surgeon fees). | Lower initial investment (existing surgical equipment), lower per-procedure costs. | Direct costs encompass all expenses directly related to the procedure itself. |
| Indirect Costs | Specialized training for surgical staff, ongoing maintenance and repair of the robotic system, potential for longer operating times (though often offset by faster recovery), increased facility infrastructure needs. | Less specialized training needed, lower maintenance costs for equipment, potentially shorter operating times (but potentially longer recovery), existing facility infrastructure sufficient. | Indirect costs include expenses related to infrastructure, training, and long-term maintenance. |
| Long-Term Costs | Potentially lower long-term costs due to reduced hospital stays, fewer complications, and faster patient recovery. | Potentially higher long-term costs due to extended hospital stays, increased risk of complications, and slower patient recovery, potentially higher readmission rates. | Long-term cost savings need to be carefully considered. Reduced complication rates and shorter hospital stays can significantly offset higher initial investment. |
Factors Influencing Accessibility of Robotic Surgery
Accessibility to robotic surgery is significantly influenced by socioeconomic factors. High initial capital costs for robotic systems often restrict access in lower-income countries and underserved communities. Moreover, the need for specialized surgical training and ongoing maintenance further limits availability. Insurance coverage also plays a crucial role, with variations in reimbursement policies impacting patient access. For example, a patient with limited or no insurance coverage in a country without substantial government subsidies might find robotic surgery financially inaccessible, even if the procedure could offer better outcomes. In contrast, patients in countries with robust healthcare systems and comprehensive insurance coverage might have more accessible options.
Strategies for Improving Cost-Effectiveness and Accessibility
Several strategies can enhance the cost-effectiveness and accessibility of robotic surgery globally. These include exploring innovative financing models, such as public-private partnerships and leasing agreements, to reduce the initial financial burden on healthcare institutions. Furthermore, developing standardized training programs and fostering collaboration among surgeons can improve the efficiency and cost-effectiveness of robotic surgery training. Finally, focusing on the development of more affordable robotic surgical systems and prioritizing access in underserved communities are essential steps towards ensuring equitable access to this life-improving technology. For instance, the development of smaller, more portable robotic systems could significantly reduce the infrastructure requirements and make robotic surgery more accessible in rural or remote areas.
Illustrative Examples
Source: oncolifehospitals.com
Real-world applications showcase the transformative impact of robotic surgery. Examining both successful and challenging cases illuminates the technology’s potential and limitations, offering valuable insights for surgeons and patients alike. These examples highlight the precision, safety improvements, and complexities inherent in robotic-assisted procedures.
Successful robotic surgery relies on meticulous planning, precise execution, and a skilled surgical team. The benefits extend beyond mere technical proficiency, impacting patient recovery and long-term outcomes.
Successful Robotic Prostatectomy
A 62-year-old male patient presented with localized prostate cancer. Traditional open prostatectomy was considered too invasive given his age and overall health. Robotic-assisted laparoscopic prostatectomy was chosen. The surgeon, using the da Vinci Surgical System, performed a minimally invasive procedure with excellent visualization and dexterity. The small incisions resulted in significantly reduced blood loss compared to open surgery (estimated 50ml vs 250ml). The patient experienced minimal post-operative pain, a shorter hospital stay (2 days vs 7 days), and a faster return to normal activities. This case demonstrates the advantages of robotic surgery in minimizing trauma, accelerating recovery, and improving the patient’s quality of life. The precise movements of the robotic arms allowed for the removal of the prostate with minimal damage to surrounding tissues, a crucial factor in preserving urinary and sexual function.
Challenging Robotic Gastrectomy
A 70-year-old female patient with a large, complex gastric tumor presented for a robotic-assisted gastrectomy. The tumor’s location and size posed significant challenges, requiring intricate dissection near vital blood vessels and organs. During the procedure, unexpected bleeding occurred near the splenic artery, necessitating quick thinking and precise adjustments by the surgical team. The surgeon skillfully used the robotic system’s enhanced visualization and articulation to control the bleeding and complete the resection. The procedure, while more complex than initially anticipated, was successfully completed.
The challenges encountered highlighted the importance of comprehensive pre-operative planning, intraoperative adaptability, and the availability of experienced surgical personnel. This case underscores the need for robust training and contingency plans in complex robotic procedures.
- Thorough pre-operative imaging and planning are crucial to anticipate and mitigate potential intraoperative complications.
- Real-time adaptability and problem-solving skills are essential for managing unforeseen circumstances.
- A highly skilled surgical team, including experienced robotic surgeons and support staff, is vital for success.
- The availability of advanced imaging and monitoring technologies enhances surgical precision and safety.
Robotic-Assisted Coronary Artery Bypass Grafting (CABG) – Internal Mammary Artery Harvesting
Imagine a detailed, three-dimensional view of the patient’s chest cavity. The surgeon, using the robotic arms, delicately dissects the internal mammary artery (IMA), a vital blood vessel used in CABG procedures. The robotic instruments provide unparalleled precision and stability, allowing the surgeon to meticulously separate the IMA from surrounding tissues with minimal trauma. The enhanced dexterity allows for precise dissection even in confined spaces, minimizing the risk of injury to adjacent structures such as the phrenic nerve or internal thoracic vein. Compared to traditional open-chest harvesting, the robotic approach results in smaller incisions, less post-operative pain, and a faster recovery time. The superior visualization allows for better identification and preservation of delicate structures, potentially leading to improved graft patency and long-term outcomes. The robotic instruments’ tremor-free movements minimize the risk of damaging the artery, improving the quality of the harvested graft.
Final Wrap-Up
The integration of robotics in surgery is not just a technological marvel; it’s a paradigm shift in patient care. While challenges remain regarding cost and accessibility, the enhanced precision, reduced complications, and improved recovery times offered by robotic surgery are undeniable. As technology continues to advance, the future of surgery looks brighter, more precise, and ultimately, safer for patients worldwide. The journey into this brave new world of surgical robotics is just beginning.
