The Future of Wearable Devices in Preventative Healthcare is brighter than ever. Imagine a world where tiny sensors on your wrist predict heart attacks before they happen, or subtly monitor your blood sugar, keeping diabetes at bay. This isn’t science fiction; it’s the rapidly evolving reality of wearable technology, promising a revolution in how we approach health and wellness. This exploration delves into the advancements, challenges, and incredible potential of wearable devices in proactively safeguarding our health.
From sophisticated sensors that track everything from heart rate variability to sleep patterns, to powerful algorithms that analyze the data and predict potential health risks, the possibilities are staggering. We’ll examine how this technology is being applied to tackle major health concerns like cardiovascular disease and diabetes, while also discussing the crucial aspects of data privacy, user experience, and seamless integration with existing healthcare systems. The journey ahead is paved with both exciting innovations and ethical considerations, a landscape we’ll navigate together.
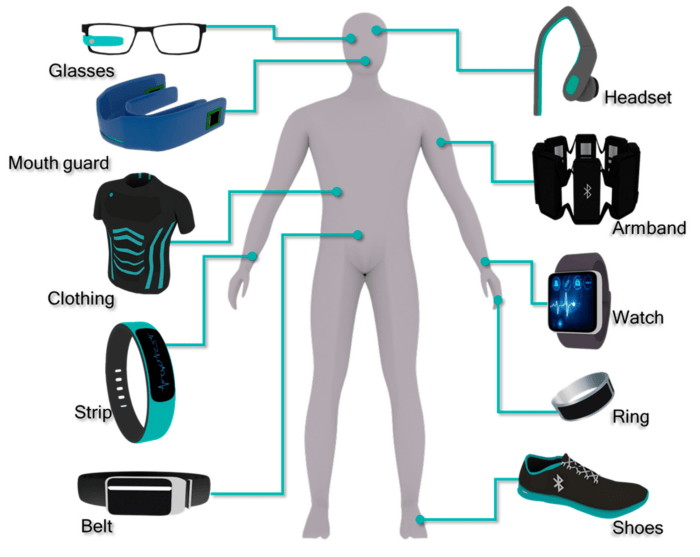
Technological Advancements in Wearable Sensors
Source: mdpi.com
Wearable tech’s future in preventative healthcare is bright, promising personalized insights and early disease detection. This personalized data boom fuels the need for smarter ad targeting, and that’s where AI comes in; check out how AI is changing the game in How AI is Changing the Future of Digital Advertising. Ultimately, this refined targeting helps deliver crucial health information directly to those who need it most, improving the effectiveness of preventative healthcare initiatives powered by wearable data.
The evolution of wearable sensors has been nothing short of revolutionary, transforming from bulky, power-hungry devices to incredibly small, energy-efficient, and highly accurate instruments. This miniaturization, coupled with advancements in processing power and wireless communication, has unlocked unprecedented opportunities for preventative healthcare. The ability to continuously monitor vital signs and physiological data outside of clinical settings is changing how we approach health management.
The miniaturization of sensors is driven by the relentless pursuit of smaller, more comfortable, and less obtrusive devices. This has involved breakthroughs in materials science, allowing for the creation of incredibly small and flexible sensors that can conform to the human body. Simultaneously, advancements in low-power electronics have enabled longer battery life, eliminating the constant need for recharging and enhancing user compliance. Improved signal processing algorithms have also significantly increased the accuracy and reliability of the data collected, leading to more accurate diagnoses and personalized health interventions.
Sensor Types in Preventative Healthcare
Wearable devices utilize a variety of sensors to gather diverse physiological data relevant to preventative healthcare. Each sensor type offers unique capabilities and limitations, necessitating careful consideration when selecting devices for specific health applications.
| Sensor Type | Capabilities | Limitations | Health Conditions Detected |
|---|---|---|---|
| Electrocardiogram (ECG) | Detects heart rhythm irregularities, such as atrial fibrillation and bradycardia. | Can be susceptible to noise and motion artifacts; accuracy may vary depending on placement and skin contact. | Atrial fibrillation, bradycardia, tachycardia, heart attacks (potential early warning signs) |
| Photoplethysmography (PPG) | Measures heart rate, blood oxygen saturation (SpO2), and blood volume pulse. | Accuracy can be affected by motion, skin pigmentation, and ambient light. Less precise than ECG for arrhythmia detection. | Heart rate variability changes, sleep apnea (potential early warning signs), hypoxia |
| Accelerometer | Tracks movement, posture, and activity levels. Can detect falls and assess physical activity. | Limited in its ability to detect subtle movements or specific physiological changes. | Sedentary lifestyle, risk of falls, potential for early detection of Parkinson’s disease symptoms (e.g., gait changes) |
| Gyroscope | Measures rotational movement, providing additional context to accelerometer data. Useful for gait analysis and fall detection. | Similar limitations to accelerometers; accuracy can be impacted by environmental factors. | Improved accuracy in fall detection, assessment of balance and coordination issues |
| Blood Glucose Sensor (Continuous Glucose Monitor – CGM) | Provides continuous monitoring of blood glucose levels. | Requires calibration; accuracy can vary depending on sensor placement and individual factors. Requires invasive insertion. | Diabetes management, early detection of hypoglycemia or hyperglycemia |
Data Analysis and Interpretation in Preventative Healthcare: The Future Of Wearable Devices In Preventative Healthcare
The deluge of data generated by wearable health devices presents both a massive opportunity and a significant challenge for preventative healthcare. Turning this raw information into actionable insights requires sophisticated data analysis and interpretation techniques, coupled with robust security measures to protect sensitive personal information. The ability to effectively process and understand this data is crucial for developing personalized preventative strategies and improving overall health outcomes.
The sheer volume and complexity of data from wearable sensors demand advanced analytical methods. Traditional statistical methods are often insufficient to uncover subtle patterns and correlations within the data streams. This is where machine learning steps in, providing powerful tools for identifying trends, predicting risks, and personalizing interventions. Algorithms ranging from simple linear regression to complex deep learning models are employed, depending on the specific application and the nature of the data. For example, recurrent neural networks (RNNs) are particularly well-suited for analyzing time-series data, like heart rate variability over time, while support vector machines (SVMs) can be effective in classifying different health states based on various sensor inputs.
Methods for Processing and Analyzing Wearable Health Data
Data preprocessing is a critical first step, involving cleaning, transforming, and preparing the raw sensor data for analysis. This might include handling missing values, smoothing noisy signals, and converting data into a suitable format for the chosen analytical method. Feature engineering, the process of creating new features from existing ones, is also crucial. For instance, deriving metrics like average heart rate, sleep duration, or activity levels from raw accelerometer and heart rate data allows for more insightful analysis. Subsequently, the selected machine learning algorithm is trained on a labeled dataset, allowing it to learn patterns and relationships within the data. Finally, the trained model is used to make predictions or classifications on new, unseen data, providing personalized insights for preventative healthcare.
Challenges in Ensuring Data Privacy and Security
The sensitive nature of health data necessitates robust security and privacy measures. Data breaches can have severe consequences, leading to identity theft, discrimination, and even harm to individuals. Several challenges exist in this area. Firstly, the decentralized nature of data collection—data residing on various devices and platforms—complicates the implementation of consistent security protocols. Secondly, the sheer volume of data increases the computational cost and complexity of encryption and other security measures. Thirdly, ensuring compliance with evolving data privacy regulations, such as GDPR and HIPAA, is a significant ongoing task. Implementing strong encryption, anonymization techniques, and robust access control mechanisms are vital to mitigate these risks. Furthermore, transparent data governance policies and user consent mechanisms are crucial for building trust and maintaining ethical data handling practices.
Translating Raw Sensor Data into Actionable Insights
The process of transforming raw sensor data into actionable insights for preventative healthcare involves several key steps:
- Data Collection: Gathering data from wearable sensors, ensuring data quality and completeness.
- Data Preprocessing: Cleaning, transforming, and preparing the data for analysis, handling missing values and noise.
- Feature Engineering: Creating new features from raw data to enhance analytical insights, such as calculating average daily steps or sleep efficiency.
- Model Selection and Training: Choosing appropriate machine learning algorithms (e.g., linear regression, random forests, neural networks) and training them on labeled datasets.
- Model Evaluation and Validation: Assessing the model’s performance using appropriate metrics and ensuring its generalizability to new data.
- Insight Generation: Using the trained model to analyze new data and generate personalized insights, such as identifying individuals at risk of developing specific health conditions.
- Intervention and Feedback: Providing personalized recommendations and feedback to users based on the generated insights, encouraging proactive health management.
Applications in Specific Health Conditions
Wearable technology is rapidly transforming preventative healthcare, moving beyond simple fitness tracking to offer sophisticated tools for early detection and management of various health conditions. The ability to continuously monitor vital signs and behavioral patterns provides invaluable data for personalized interventions, potentially revolutionizing how we approach chronic diseases. This section explores the applications of wearable devices in preventing cardiovascular disease, diabetes, and mental health issues, acknowledging both their potential and limitations.
The integration of wearable sensors with sophisticated algorithms allows for the continuous monitoring of physiological parameters, paving the way for early intervention strategies. This proactive approach stands in stark contrast to traditional reactive healthcare models, which often address issues only after symptoms become apparent. The potential for improved health outcomes and reduced healthcare costs is significant, particularly in managing prevalent chronic diseases.
Wearable Technology in Cardiovascular Disease Prevention
Wearable devices equipped with heart rate monitors, electrocardiogram (ECG) sensors, and activity trackers are already playing a significant role in cardiovascular disease prevention. Continuous heart rate monitoring can identify irregular heart rhythms (arrhythmias), a key indicator of potential heart problems. Activity trackers encourage physical activity, a crucial factor in maintaining cardiovascular health. Furthermore, some devices can detect subtle changes in heart rate variability, providing early warnings of potential cardiac events. For instance, Apple Watch’s ECG functionality has been shown to detect atrial fibrillation, a common arrhythmia that increases the risk of stroke, allowing for timely medical intervention. However, it’s crucial to remember that these devices are not replacements for professional medical diagnoses. False positives and limitations in accuracy necessitate careful interpretation of the data and confirmation through traditional medical assessments.
Wearable Technology in Diabetes Prevention and Management
Wearable devices offer several applications in diabetes prevention and management. Continuous glucose monitors (CGMs) provide real-time glucose data, allowing individuals to make informed decisions about diet and exercise. Smartwatches can track activity levels and sleep patterns, both of which significantly impact blood glucose control. Data collected by these devices can be integrated with smartphone apps, providing users with personalized insights and recommendations. For example, studies have shown that using CGMs alongside lifestyle interventions leads to better glycemic control in individuals with type 1 and type 2 diabetes. However, the cost of CGMs can be a barrier for some, and the potential for alarm fatigue (due to frequent alerts) needs to be addressed through user-friendly interfaces and intelligent alert systems.
Wearable Technology in Mental Health, The Future of Wearable Devices in Preventative Healthcare
The application of wearable technology in mental health is still emerging but holds immense promise. Wearables can track sleep patterns, activity levels, and even subtle changes in heart rate variability, which can be indicative of stress and anxiety. This data, combined with self-reported mood data through accompanying apps, can provide a comprehensive picture of an individual’s mental well-being. For example, studies have shown that wearable-based interventions can be effective in improving mood and reducing symptoms of depression and anxiety. However, ethical considerations regarding data privacy and the potential for misuse of sensitive mental health data are paramount. Ensuring data security and obtaining informed consent are crucial to building trust and ensuring responsible use of this technology.
Integration with Existing Healthcare Systems

Source: nftevening.com
Integrating data from wearable devices into the existing healthcare ecosystem presents both significant challenges and exciting opportunities. The seamless flow of this data into electronic health records (EHRs) and other healthcare systems is crucial for realizing the full potential of preventative healthcare powered by wearables. Success hinges on overcoming interoperability issues and ensuring data privacy and security.
The successful integration of wearable data into existing healthcare systems requires a multi-faceted approach. This involves addressing technological hurdles, establishing robust data security protocols, and navigating the complex regulatory landscape surrounding patient health information. Furthermore, clinicians need to be trained to effectively interpret and utilize this new influx of data to improve patient care.
Challenges of Integrating Wearable Data into EHRs
Integrating data from wearable devices into EHRs is not without its hurdles. Data standardization is a major challenge; different devices use different formats and protocols, making it difficult to consolidate data from multiple sources into a unified view within the EHR. Ensuring data security and patient privacy is paramount, requiring robust encryption and access control mechanisms to prevent unauthorized access and data breaches. Furthermore, the sheer volume of data generated by wearable devices can strain existing EHR infrastructure, necessitating upgrades and optimization to handle the increased workload. Finally, the lack of clear clinical guidelines on how to interpret and utilize wearable data within the clinical workflow creates uncertainty and potential for misinterpretation.
Workflow Diagram for Wearable Data Integration
Imagine a patient, Sarah, who wears a smartwatch that monitors her heart rate, activity levels, and sleep patterns. This data is automatically uploaded to a secure cloud platform. The platform uses algorithms to analyze the data, flagging any potential anomalies, such as an elevated resting heart rate or decreased activity levels. These alerts are then sent to Sarah’s physician through a secure portal integrated with their EHR system. The physician reviews the data alongside Sarah’s other medical information within the EHR, allowing for a more comprehensive assessment of her health. If necessary, the physician can then initiate further investigations, such as ordering additional tests or scheduling a follow-up appointment. This streamlined process improves communication, allowing for proactive intervention and better management of Sarah’s health. The entire process is designed to be secure, ensuring patient privacy and data integrity.
Impact of Wearable Data on Healthcare Costs and Resource Allocation
The integration of wearable device data holds the potential to significantly impact healthcare costs and resource allocation. By enabling early detection of health issues, wearable technology can prevent costly hospitalizations and emergency room visits. For example, a smartwatch detecting an irregular heartbeat could prompt early intervention for atrial fibrillation, reducing the risk of stroke and associated healthcare costs. Furthermore, remote patient monitoring using wearable devices can reduce the need for frequent in-person clinic visits, freeing up healthcare professionals’ time and resources. This shift towards proactive and preventative care can lead to more efficient resource allocation and a more sustainable healthcare system. However, the initial investment in infrastructure and training is significant. The long-term cost-effectiveness will depend on widespread adoption and the development of robust, scalable systems for data analysis and integration. Studies have shown promising cost savings in specific chronic disease management using remote monitoring via wearables, suggesting a future where this technology plays a significant role in containing healthcare expenditure.
User Experience and Adoption
The success of preventative healthcare wearable devices hinges entirely on user adoption and consistent adherence. While the technology offers incredible potential, its effectiveness is drastically reduced if individuals don’t wear and engage with the devices regularly. Several intertwined factors influence whether someone embraces a wearable for their health, and understanding these is key to designing truly impactful technology.
Factors influencing user adoption and adherence are complex and multifaceted. Convenience, for instance, plays a crucial role; a device that’s uncomfortable, difficult to charge, or requires complicated setup will quickly be abandoned. Similarly, the perceived value of the data collected significantly impacts user engagement. If users don’t understand how the data benefits them or see a clear link between their actions and health improvements, motivation wanes. Privacy concerns are also paramount; users need assurance that their sensitive health data is secure and handled responsibly. Finally, the design of the device and its associated app, including ease of use and clarity of information presented, greatly influence long-term use. A poorly designed interface can lead to frustration and ultimately, abandonment.
Strategies to Improve User Engagement and Motivation
Improving user engagement requires a multi-pronged approach. Simply providing a device isn’t enough; users need ongoing support and encouragement. Effective strategies include gamification, personalized feedback, and social support features.
- Gamification: Incorporating game mechanics, such as points, badges, and leaderboards, can incentivize consistent use and healthy behaviors. For example, awarding points for achieving daily step goals or maintaining a healthy sleep schedule can foster a sense of accomplishment and motivation.
- Personalized Feedback: Providing users with clear, actionable insights based on their data is crucial. Instead of just presenting raw data, the device and app should translate it into meaningful recommendations and progress reports. For instance, an app could show a user how their sleep patterns are improving over time and suggest ways to further optimize their sleep hygiene.
- Social Support Features: Allowing users to connect with friends, family, or support groups can create a sense of community and accountability. Features such as shared challenges or progress tracking can encourage healthy competition and mutual support.
- Integration with Existing Health Platforms: Seamless integration with existing health apps and platforms (like Apple Health or Google Fit) can streamline data management and provide a more holistic view of a user’s health. This avoids data silos and enhances the overall user experience.
- Regular Updates and New Features: Keeping the device’s software updated with new features and improvements keeps users engaged and shows that the developers are committed to the product’s long-term success. This could include adding new health metrics, improving the accuracy of existing sensors, or introducing new personalized recommendations.
Ideal User Interface Design for Preventative Healthcare Wearables
The ideal user interface should prioritize simplicity, clarity, and personalization. The device itself should be comfortable and unobtrusive, seamlessly integrating into the user’s daily life. The accompanying app should present information in a visually appealing and easy-to-understand manner, focusing on key metrics and actionable insights.
The home screen could display a summary of key health metrics, such as daily steps, heart rate variability, sleep quality, and stress levels, using clear visuals like graphs and charts. Detailed views for each metric would allow users to explore their data further, identifying trends and patterns. The app could also include personalized recommendations based on the user’s data, suggesting lifestyle changes to improve their health. For example, if a user’s sleep quality is consistently low, the app could recommend adjusting their bedtime routine or creating a relaxing pre-sleep ritual. Notifications and reminders could encourage consistent engagement and prompt users to take action, such as reminding them to drink water or take their medication. The design should be customizable, allowing users to personalize their dashboards and select the metrics most relevant to their health goals. Finally, clear and accessible privacy settings should be prominently featured, empowering users to control their data and ensuring their peace of mind.
Future Trends and Predictions
The landscape of preventative healthcare is poised for a dramatic transformation in the next 5-10 years, driven by rapid advancements in wearable technology. We’re moving beyond simple fitness trackers to highly sophisticated devices capable of providing personalized insights into our health, potentially preventing serious illnesses before they even manifest. This shift will be fueled by breakthroughs in sensor technology, artificial intelligence, and materials science, creating a future where proactive health management is the norm.
Predicting the exact trajectory is challenging, but several key trends are emerging, promising a future where wearable devices play an increasingly vital role in preventing disease and improving overall well-being.
Miniaturization and Enhanced Sensor Capabilities
The next generation of wearable sensors will be smaller, more comfortable, and far more capable. Imagine a tiny, almost invisible patch that monitors a multitude of vital signs – heart rate, blood pressure, blood glucose, even subtle changes in skin temperature indicative of infection. This miniaturization will be achieved through advancements in microelectromechanical systems (MEMS) and flexible electronics, allowing for seamless integration into clothing or even implanted under the skin. The enhanced capabilities will extend to more accurate and sensitive measurements, leading to earlier and more precise detection of health anomalies. For example, we can anticipate the development of sensors that can detect early signs of cardiovascular disease or cancer through subtle changes in biomarkers present in sweat or saliva. These improvements will move us beyond simple trend tracking to real-time physiological monitoring with unprecedented accuracy.
The Synergistic Role of AI and IoMT
Artificial intelligence (AI) and the Internet of Medical Things (IoMT) will be pivotal in unlocking the full potential of wearable data. AI algorithms will analyze the massive datasets generated by wearables, identifying patterns and anomalies that might be missed by human observation. This will enable predictive analytics, allowing healthcare professionals to proactively intervene and prevent adverse health events. For instance, AI could analyze heart rate variability data from a wearable to predict an impending heart attack, allowing for timely medical intervention. IoMT will further enhance this capability by seamlessly integrating wearable data with electronic health records (EHRs) and other healthcare systems, providing a holistic view of a patient’s health. This interconnectedness will facilitate remote patient monitoring, personalized treatment plans, and improved communication between patients and their healthcare providers. Imagine a scenario where a wearable detects an irregular heartbeat, automatically alerts the patient’s doctor, and triggers a telehealth consultation, all without the patient having to actively seek medical attention.
Advancements in Materials Science and Nanotechnology
The materials used in wearable devices will significantly influence their functionality, comfort, and longevity. Advancements in materials science and nanotechnology will lead to the development of more biocompatible, flexible, and durable materials. This will pave the way for wearable sensors that are comfortable enough to be worn continuously, even during sleep or strenuous activity. Nanotechnology, in particular, offers exciting possibilities for developing highly sensitive sensors that can detect minute changes in body chemistry, leading to earlier disease detection. For example, nanomaterials could be integrated into fabrics to create “smart clothing” that continuously monitors vital signs and releases medication as needed. The development of biodegradable and self-powered sensors is also on the horizon, further enhancing the usability and sustainability of wearable technology in preventative healthcare.
Wrap-Up
Wearable technology’s role in preventative healthcare is no longer a futuristic fantasy; it’s a rapidly unfolding reality. While challenges remain in areas like data security and user adoption, the potential benefits – earlier disease detection, personalized interventions, and ultimately, healthier lives – are too significant to ignore. As sensor technology continues to miniaturize, AI algorithms become more sophisticated, and integration with healthcare systems improves, we can expect wearable devices to play an increasingly crucial role in shaping a healthier future for all. The future is wearable, and it’s preventative.
