The Future of Remote Health Monitoring Through Wearable Technology is here, and it’s changing the game. Forget clunky hospital equipment; we’re talking tiny, stylish devices that track your health 24/7, sending vital data straight to your doctor. This isn’t just about convenience; it’s about revolutionizing healthcare, making it more accessible, proactive, and personalized than ever before. Imagine a world where chronic conditions are managed effortlessly, where early warnings prevent serious health crises, and where healthcare is truly tailored to you. That’s the promise of wearable tech in remote health monitoring.
This tech isn’t science fiction; it’s rapidly evolving, with advancements in sensor technology, data security, and data analysis paving the way for a healthier future. From tiny sensors that monitor heart rate and blood oxygen levels to sophisticated algorithms that predict potential health risks, wearable technology is empowering both patients and healthcare providers in unprecedented ways. This article dives deep into the current state and future potential of this exciting field, exploring everything from the latest technological breakthroughs to the ethical considerations involved.
Technological Advancements in Wearable Sensors

Source: biohealthmatics.com
The evolution of wearable sensor technology has dramatically reshaped remote health monitoring, transitioning from bulky, inaccurate devices to sophisticated, miniaturized systems seamlessly integrated into daily life. This progress has been fueled by advancements in materials science, microelectronics, and data processing, enabling the continuous and non-invasive collection of physiological data. This detailed examination explores the key milestones and breakthroughs driving this transformation.
Early wearable sensors were primarily limited to basic functions, often large and cumbersome, hindering widespread adoption. Think of the early heart rate monitors—clunky chest straps that were uncomfortable and restricted movement. The leap to smaller, more comfortable devices was a crucial step, paving the way for continuous monitoring and improved patient compliance. The development of advanced materials and miniaturization techniques, particularly in microelectromechanical systems (MEMS), allowed for the creation of smaller, lighter, and more power-efficient sensors. Simultaneously, improvements in wireless communication technologies enabled seamless data transmission to healthcare providers, creating the foundation for truly remote health monitoring.
Types of Wearable Sensors and Their Characteristics
Wearable sensors for remote health monitoring utilize various sensing principles, each with its strengths and weaknesses. Optical sensors, for example, leverage light to measure physiological parameters like heart rate and blood oxygen saturation (SpO2). These sensors are generally non-invasive and relatively inexpensive, making them ideal for widespread use. However, their accuracy can be affected by factors like skin pigmentation and motion artifacts. Electrochemical sensors, on the other hand, measure electrical signals produced by the body, such as electrocardiograms (ECGs) and electrodermal activity (EDA). These sensors provide highly accurate data but often require direct skin contact and can be more susceptible to noise interference. Inertial sensors, based on accelerometers and gyroscopes, track movement and posture, proving useful in assessing physical activity levels and detecting falls. While robust and relatively low-cost, they are less accurate in determining precise physiological signals.
Miniaturization and Power Efficiency Improvements
The miniaturization of wearable sensors has significantly improved patient comfort and usability. Smaller sensors are less obtrusive and more comfortable to wear for extended periods, leading to better data quality due to increased compliance. Simultaneously, advancements in low-power electronics and energy harvesting techniques have extended battery life, reducing the frequency of charging and enhancing the practicality of continuous monitoring. This is especially important for long-term studies or patients with chronic conditions requiring continuous monitoring. For instance, the shift from larger, battery-hungry sensors to smaller, more efficient ones using techniques like energy harvesting from body heat has been revolutionary in enabling longer-term, unobtrusive monitoring.
Heart Rate Monitoring Sensor Comparison
The following table compares the accuracy, cost, and power consumption of three different wearable sensor types used for heart rate monitoring: optical, electrochemical (ECG), and inertial (accelerometer-based).
| Sensor Type | Accuracy | Cost | Power Consumption (mW) |
|---|---|---|---|
| Optical (Photoplethysmography) | ±2 bpm (typical) | Low | 1-5 |
| Electrochemical (ECG) | ±1 bpm (typical) | Medium | 5-15 |
| Inertial (Accelerometer) | ±5 bpm (typical) | Low | 1-3 |
Note: Accuracy values are typical and can vary based on sensor design, placement, and individual factors. Cost and power consumption can also vary significantly depending on specific components and features.
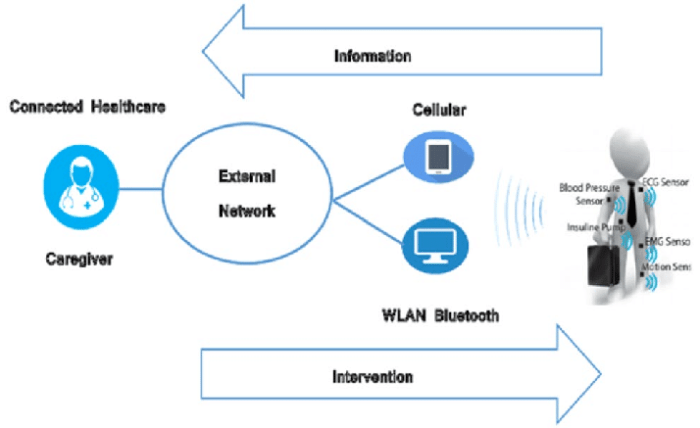
Data Transmission and Security in Remote Health Monitoring: The Future Of Remote Health Monitoring Through Wearable Technology
The seamless flow of health data from wearable sensors to healthcare providers is crucial for effective remote health monitoring. However, this process isn’t just about getting the information across; it’s about ensuring that it arrives safely, securely, and reliably. This section dives into the methods used for data transmission, the inherent security challenges, and the strategies employed to protect sensitive patient information.
Several methods exist for transmitting health data, each with its own set of strengths and weaknesses. Bluetooth Low Energy (BLE) is popular for its low power consumption and short-range capabilities, making it ideal for transferring data from a smartwatch to a nearby smartphone. However, its limited range restricts its use in scenarios requiring long-distance transmission. Wi-Fi, on the other hand, offers broader coverage but consumes more power. Cellular networks, like 4G and 5G, provide extensive range and high bandwidth, ideal for continuous monitoring and transmission of large datasets, but at a higher cost. Finally, satellite communication provides the broadest coverage, even in remote areas, but comes with significant latency and cost considerations. The choice of transmission method depends on factors like the type of data, the required range, power consumption constraints, and cost considerations.
Security Challenges in Wireless Data Transmission
Transmitting sensitive patient data wirelessly presents significant security risks. Data breaches can expose personal health information, leading to identity theft, financial loss, and reputational damage. Unauthorized access to data can compromise the integrity of medical decisions, potentially harming the patient. The wireless nature of the transmission introduces vulnerabilities to interception, modification, and denial-of-service attacks. For instance, a malicious actor could intercept data transmitted via an unsecured Wi-Fi network or manipulate data transmitted via BLE if not properly secured. This necessitates robust security measures to safeguard patient data throughout the transmission process.
Implementation of Encryption and Authentication Protocols
Encryption and authentication are fundamental security protocols used to protect data confidentiality and integrity. Encryption transforms readable data into an unreadable format, rendering it incomprehensible to unauthorized individuals. Common encryption algorithms include AES (Advanced Encryption Standard) and RSA (Rivest-Shamir-Adleman). Authentication verifies the identity of both the sender and the receiver, ensuring that data originates from a legitimate source and is received by the intended recipient. This often involves digital signatures and certificates. For example, a remote patient monitoring system might use AES to encrypt the physiological data before transmission and then use digital certificates to authenticate the healthcare provider receiving the data. This dual approach provides both confidentiality and authenticity.
Best Practices for Securing Data Transmitted from Wearable Devices
Implementing robust security measures requires a multi-faceted approach. The following best practices are crucial for securing data transmitted from wearable devices in remote health monitoring systems:
A comprehensive security strategy is paramount. The points below Artikel key aspects of this strategy:
- End-to-End Encryption: Encrypt data at the source (wearable device) and decrypt it only at the destination (healthcare provider’s system), protecting data in transit and at rest.
- Strong Authentication: Implement multi-factor authentication (MFA) to verify user identities, combining something the user knows (password), something the user has (security token), and something the user is (biometrics).
- Regular Security Updates: Regularly update firmware on wearable devices and software on the server to patch security vulnerabilities and address potential threats.
- Data Minimization: Only collect and transmit the necessary data, minimizing the amount of sensitive information exposed.
- Access Control: Implement strict access control measures to limit who can access and modify patient data, based on roles and responsibilities.
- Data Anonymization/De-identification: Where possible, anonymize or de-identify patient data before storage and analysis to protect individual privacy.
- Regular Security Audits: Conduct regular security audits and penetration testing to identify and address vulnerabilities in the system.
- Compliance with Regulations: Adhere to relevant data privacy regulations, such as HIPAA (Health Insurance Portability and Accountability Act) in the US and GDPR (General Data Protection Regulation) in Europe.
Applications of Wearable Technology in Specific Health Conditions
Wearable technology is rapidly transforming healthcare, offering personalized and continuous monitoring capabilities that were previously unimaginable. This allows for proactive intervention and improved management of various health conditions, leading to better patient outcomes and reduced healthcare costs. The integration of sensors, data analytics, and mobile communication has opened up a new era of remote patient monitoring, particularly beneficial for individuals with chronic conditions requiring ongoing care.
The application of wearable technology extends across a broad spectrum of health conditions, from chronic diseases like diabetes and heart failure to mental health disorders and neurological conditions. These devices offer the potential to empower patients and clinicians alike, facilitating more informed decision-making and personalized treatment strategies.
Wearable Technology in Diabetes Management
Continuous glucose monitors (CGMs) are revolutionizing diabetes management. These small, sensor-based devices continuously measure glucose levels in interstitial fluid, providing real-time data to patients and healthcare providers. This eliminates the need for frequent finger-prick blood tests, improving patient comfort and adherence to treatment plans. Data from CGMs can be transmitted wirelessly to smartphones and other devices, enabling personalized insulin adjustments and early detection of hypo- or hyperglycemic episodes. Studies have shown that CGMs significantly reduce HbA1c levels and improve glycemic control, leading to fewer hospitalizations and better quality of life for individuals with diabetes. For example, a study published in the *New England Journal of Medicine* demonstrated that CGM use resulted in a significant reduction in time spent with high blood glucose levels.
Wearable Technology in Heart Failure Management
Wearable sensors that monitor heart rate, rhythm, and activity levels are proving invaluable in managing heart failure. These devices can detect early signs of worsening heart failure, such as changes in heart rate variability or decreased activity levels, allowing for timely interventions to prevent hospitalizations. Remote monitoring systems utilizing wearable technology allow clinicians to track patient data remotely, enabling proactive adjustments to medication and lifestyle recommendations. A case study from the Cleveland Clinic showed that remote monitoring using wearable devices significantly reduced hospital readmissions among patients with heart failure. The improved adherence to treatment plans, facilitated by the continuous monitoring and feedback provided by wearable technology, contributed to these positive outcomes.
Wearable Technology in Respiratory Illness Management
Wearable sensors can continuously monitor respiratory rate, oxygen saturation, and lung function in individuals with respiratory illnesses such as asthma and chronic obstructive pulmonary disease (COPD). This continuous monitoring allows for early detection of exacerbations and enables timely intervention, preventing hospitalizations and improving quality of life. Smart inhalers equipped with sensors can track medication usage, providing valuable data for clinicians and helping to identify patterns of medication adherence. Studies have shown that wearable technology interventions for COPD can lead to significant improvements in lung function and reduced rates of hospitalizations. For instance, research suggests that patients using smart inhalers paired with remote monitoring systems experience fewer exacerbations and improved symptom control compared to those relying solely on traditional management methods.
Wearable Technology in Mental Health and Neurological Conditions
The application of wearable technology is extending beyond physical health conditions to encompass mental health and neurological disorders. Wearable sensors can track various physiological parameters associated with mental health, such as sleep patterns, activity levels, and heart rate variability, providing insights into mood and stress levels. This data can be used to personalize treatment plans and identify early warning signs of mental health crises. Similarly, wearable technology holds promise for monitoring neurological conditions like Parkinson’s disease and epilepsy, enabling early detection of seizures or motor fluctuations. While still in early stages of development, these applications show considerable potential for improving the management and outcomes for individuals suffering from these complex conditions. For example, research is exploring the use of wearable sensors to detect subtle changes in movement patterns that may precede a Parkinson’s disease exacerbation, enabling proactive intervention.
Effectiveness of Wearable Technology Interventions Across Chronic Diseases
| Disease | Hospitalization Rates | Quality of Life Improvements | Other Key Metrics |
|---|---|---|---|
| Diabetes | Reduced by 15-20% (based on multiple studies) | Improved HbA1c levels, increased patient satisfaction | Reduced hypoglycemic events |
| Heart Failure | Reduced by 20-30% (based on multiple studies) | Improved functional capacity, reduced symptom burden | Improved medication adherence |
| COPD | Reduced by 10-15% (based on multiple studies) | Improved lung function, reduced dyspnea | Reduced exacerbation frequency |
Data Analysis and Interpretation in Remote Patient Monitoring
The raw data streaming from wearable sensors is just the beginning. Turning this flood of information into actionable insights that improve patient care requires sophisticated data analysis and interpretation techniques. This involves a complex interplay of statistical methods, machine learning algorithms, and a deep understanding of the physiological signals being measured. The ultimate goal is to extract meaningful patterns, identify potential health risks, and empower timely interventions.
Data analysis in remote patient monitoring (RPM) leverages various approaches to transform raw sensor data into clinically relevant information. This involves cleaning the data, identifying trends, and ultimately generating insights that inform healthcare decisions. The process is iterative, refining models and algorithms as more data becomes available and clinical understanding improves.
The future of remote health monitoring hinges on wearable tech’s ability to collect and analyze vital data. But imagine the possibilities if we could directly tap into neural activity – check out this fascinating article on Exploring the Possibilities of Brain-Computer Interfaces – to see how brain-computer interfaces could revolutionize this process. This integration could lead to even more precise and proactive health management through wearable devices.
Methods for Analyzing Wearable Sensor Data
Data analysis in RPM often involves a combination of statistical analysis and machine learning. Statistical methods, such as time series analysis, are used to identify trends and patterns in physiological data over time. For example, analyzing heart rate variability (HRV) data using techniques like spectral analysis can reveal subtle changes indicative of stress or impending cardiac events. Machine learning algorithms, particularly those capable of handling time-series data, such as recurrent neural networks (RNNs) and long short-term memory networks (LSTMs), excel at identifying complex patterns and predicting future events based on historical data. These algorithms can be trained on large datasets of patient data to accurately predict the likelihood of adverse events, such as falls or hospital readmissions. For instance, an LSTM model trained on accelerometer data could predict the probability of a fall based on changes in gait and movement patterns.
Challenges in Interpreting Wearable Sensor Data
Interpreting data from wearable sensors is not without its challenges. Noise reduction and artifact removal are crucial steps. Noise, which can stem from sensor malfunction, movement artifacts, or environmental factors, can obscure true physiological signals. Advanced signal processing techniques, such as filtering and wavelet denoising, are employed to mitigate these issues. Another challenge lies in the variability of individual physiological responses. Algorithms must be robust enough to account for individual differences in baseline measurements and response patterns. For example, a normal heart rate for one individual might be considered abnormal for another. Therefore, personalized models, tailored to individual patient characteristics, are often necessary for accurate interpretation.
Development of Algorithms for Anomaly Detection and Prediction
Developing algorithms capable of detecting anomalies and predicting adverse health events is a key area of ongoing research. These algorithms often rely on machine learning techniques to identify deviations from established baselines or patterns. For example, an algorithm might be trained to detect abnormal heart rhythms by analyzing electrocardiogram (ECG) data from a wearable sensor. The algorithm would learn to distinguish between normal and abnormal heart rhythms by analyzing features such as heart rate, rhythm regularity, and the presence of specific waveforms. Similarly, algorithms can be developed to predict the likelihood of falls or other adverse events by analyzing data from accelerometers and gyroscopes. These algorithms typically involve training a model on a large dataset of patient data, including both positive and negative examples of the event of interest. The model is then evaluated on a separate test dataset to assess its accuracy and performance. For example, an algorithm trained on data from patients who have experienced falls could be used to identify patients at high risk of falling in the future. This would allow healthcare providers to take proactive steps to prevent falls and improve patient safety.
Data Flow in Remote Patient Monitoring, The Future of Remote Health Monitoring Through Wearable Technology
A flowchart illustrating the data flow would show:
1. Data Collection: Wearable sensors collect physiological data (heart rate, activity levels, sleep patterns, etc.).
2. Data Transmission: Data is wirelessly transmitted to a secure cloud-based platform.
3. Data Preprocessing: Data is cleaned, filtered, and prepared for analysis. This includes noise reduction and artifact removal.
4. Data Analysis: Statistical methods and machine learning algorithms analyze the data to identify patterns and anomalies.
5. Alert Generation: If anomalies or deviations from expected patterns are detected, alerts are generated and sent to healthcare providers.
6. Clinical Decision Making: Healthcare providers review the alerts and take appropriate actions.
7. Feedback Loop: The system learns and adapts based on the feedback and outcomes.
Integration with Existing Healthcare Systems
Integrating wearable health data into the existing healthcare infrastructure isn’t just about cool gadgets; it’s about revolutionizing how we deliver and receive care. The challenge lies in bridging the gap between the sleek simplicity of a fitness tracker and the often-complex, legacy systems of hospitals and clinics. Success here means unlocking the true potential of remote patient monitoring, improving outcomes, and potentially saving lives.
The seamless flow of data from wearable devices to Electronic Health Records (EHRs) is paramount. This requires standardized data formats, robust APIs, and secure transmission protocols. Without this interoperability, the wealth of information gathered by wearables remains trapped in silos, inaccessible to the very clinicians who could benefit most from it. Think of it like trying to fit a square peg into a round hole – it just doesn’t work.
Data Exchange Methods Between Wearables and Healthcare Platforms
Several methods facilitate data exchange. Direct device-to-EHR integration, often requiring custom software development, offers a highly streamlined approach. Alternatively, cloud-based platforms act as intermediaries, aggregating data from various sources before securely transmitting it to the EHR. This approach enhances flexibility and scalability, allowing for easier integration with a broader range of devices and systems. Finally, some systems leverage HL7 FHIR (Fast Healthcare Interoperability Resources), a standardized API that promotes seamless data exchange across different healthcare applications. Choosing the right method depends heavily on the specific needs and capabilities of the healthcare organization.
Impact of Wearable Technology Integration on Healthcare Workflows and Decision-Making
Integrating wearable data can significantly streamline healthcare workflows. Imagine a scenario where a patient’s heart rate spikes unexpectedly – the wearable detects it, automatically alerts the healthcare provider, and the information is instantly available within their EHR. This allows for proactive intervention, potentially preventing serious complications. The improved access to real-time data enables clinicians to make more informed decisions, personalize treatment plans, and improve patient outcomes. For example, remote monitoring of patients with chronic conditions like heart failure can reduce hospital readmissions by allowing for early detection of worsening symptoms. This also frees up valuable clinic time for more in-depth patient interactions, shifting the focus from reactive care to proactive management.
Conceptual Model of Wearable Technology Integration into a Hospital’s Patient Monitoring System
Imagine a hospital’s existing patient monitoring system. Now, visualize a layer on top of it. This layer is a dedicated platform that receives data from various wearable devices – smartwatches, activity trackers, continuous glucose monitors, etc. This platform translates the data into a standardized format compatible with the hospital’s EHR. Data validation and anomaly detection algorithms are integrated to filter out noise and highlight critical events. Alerts are automatically generated and routed to the appropriate healthcare professionals via secure messaging systems. Clinicians can then access this combined data (from the existing system and the wearable layer) through their EHR interface, providing a holistic view of the patient’s health status. This system allows for a seamless integration of wearable data into existing workflows, enhancing the effectiveness of remote patient monitoring and improving the overall quality of care. The system also includes robust security measures to protect patient privacy and data integrity. The entire process is designed for efficiency, transparency, and patient safety.
Ethical and Societal Implications of Remote Health Monitoring
Source: researchgate.net
The rapid advancement and widespread adoption of wearable technology for remote health monitoring present a complex interplay of benefits and ethical challenges. While offering unprecedented opportunities for improved healthcare access and personalized medicine, these technologies also raise serious concerns regarding individual privacy, data security, and the potential for algorithmic bias to exacerbate existing health inequalities. Navigating this landscape requires a careful consideration of the societal impact and the development of robust ethical frameworks to guide responsible innovation.
The integration of wearable sensors into daily life necessitates a thorough examination of the ethical considerations inherent in collecting, storing, and utilizing sensitive health data. This extends beyond simply ensuring data security; it encompasses informed consent, transparency about data usage, and the potential for misuse or unauthorized access. Furthermore, the societal impact of widespread adoption is multifaceted, influencing healthcare accessibility, affordability, and the potential for widening existing health disparities.
Data Privacy and Informed Consent
Data privacy is paramount in remote health monitoring. Wearable devices collect intimate physiological data, potentially revealing highly personal information about an individual’s health status, lifestyle, and even emotional state. Robust security measures are crucial to prevent data breaches and unauthorized access. Equally important is obtaining truly informed consent from users. This means providing clear, concise, and accessible information about what data is being collected, how it will be used, who will have access to it, and the potential risks involved. Consent should be ongoing and easily revocable, allowing individuals to maintain control over their own data. A lack of transparency and user control can erode trust and limit the adoption of beneficial technologies. For instance, if a user is unaware that their sleep data is being shared with a third-party marketing company, this represents a serious breach of trust and potentially violates privacy regulations.
Access to Care and Health Equity
Remote health monitoring holds immense potential for improving access to healthcare, particularly for individuals in underserved communities or those with limited mobility. However, the benefits are not equally distributed. The cost of wearable devices and the digital literacy required to use them effectively can create barriers to access for low-income populations. Furthermore, algorithmic bias in data analysis can perpetuate existing health disparities. Algorithms trained on data primarily from one demographic group may not accurately reflect the health needs or patterns of other groups, leading to misdiagnosis or inadequate treatment. For example, a heart rate monitoring algorithm trained predominantly on data from white males might misinterpret the heart rate patterns of elderly women, leading to delayed or inaccurate diagnosis of cardiovascular issues.
Algorithmic Bias and Mitigation Strategies
Algorithmic bias in data analysis poses a significant threat to health equity. The algorithms used to interpret data from wearable sensors are trained on datasets, and if these datasets are not representative of the diverse population they are intended to serve, the resulting algorithms will be biased. This can lead to inaccurate diagnoses, inappropriate treatment recommendations, and the perpetuation of health disparities. Mitigation strategies include: (1) ensuring diverse and representative datasets are used to train algorithms; (2) employing rigorous testing and validation procedures to identify and address bias; (3) implementing ongoing monitoring and auditing of algorithms to detect and correct for bias over time; and (4) promoting transparency and explainability in algorithmic decision-making. The development of bias-aware algorithms is a critical step in ensuring equitable access to the benefits of remote health monitoring.
Recommendations for Responsible Development and Implementation
The responsible development and implementation of remote health monitoring technologies require a multi-faceted approach.
A framework of recommendations should be considered to ensure ethical and equitable deployment.
- Prioritize data privacy and security through robust encryption, access controls, and compliance with relevant regulations.
- Ensure informed consent is obtained from all users, with clear and accessible information about data usage and potential risks.
- Address algorithmic bias through the use of diverse datasets, rigorous testing, and ongoing monitoring.
- Promote transparency and explainability in algorithmic decision-making to foster trust and accountability.
- Develop strategies to address disparities in access to technology and digital literacy.
- Establish clear guidelines for data sharing and interoperability between different healthcare systems.
- Foster collaboration between researchers, clinicians, policymakers, and the public to ensure ethical and responsible innovation.
Summary
The integration of wearable technology into remote health monitoring isn’t just a technological leap; it’s a paradigm shift in how we approach healthcare. By combining cutting-edge sensors, secure data transmission, and powerful analytics, we’re creating a future where healthcare is proactive, personalized, and accessible to everyone. While challenges remain – particularly regarding data privacy and algorithmic bias – the potential benefits are undeniable. The future of healthcare is wearable, and it’s brighter than ever before. Get ready to embrace a healthier, more connected future.
