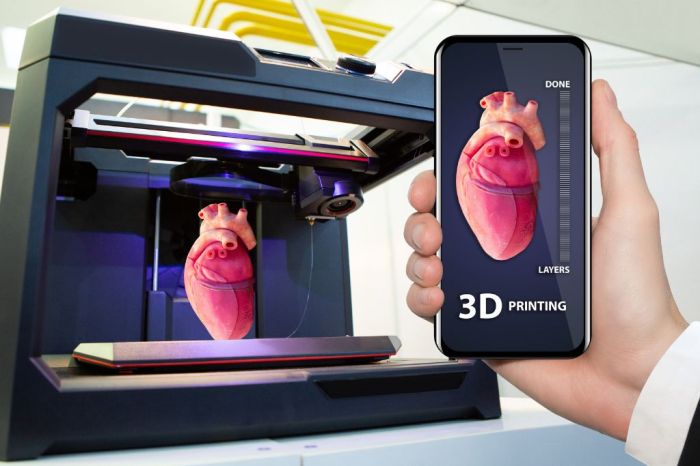
The Future of 3D Printing in Advancing Medical Research is exploding. Imagine personalized medicine where implants are custom-built for your body, drugs are delivered precisely where they’re needed, and even organs are grown on demand. This isn’t science fiction; it’s the incredible potential of 3D printing in revolutionizing healthcare, from creating patient-specific treatments to accelerating drug discovery. We’re diving deep into how this technology is shaping the future of medical breakthroughs.
From bioprinting intricate tissues to developing innovative biomaterials and streamlining drug development, 3D printing is proving to be a game-changer. This article explores the cutting-edge advancements, the hurdles yet to overcome, and the ethical considerations that accompany this revolutionary technology. Get ready to be amazed by the potential of this rapidly evolving field.
Personalized Medicine and 3D Printing
The convergence of 3D printing and personalized medicine is revolutionizing healthcare, offering unprecedented opportunities to tailor treatments to individual patients. This approach moves beyond the “one-size-fits-all” model, allowing for more effective and precise interventions. By leveraging the capabilities of additive manufacturing, we can create customized medical solutions that address the unique needs of each individual.
3D Bioprinting of Patient-Specific Implants and Prosthetics, The Future of 3D Printing in Advancing Medical Research
3D bioprinting allows for the creation of patient-specific implants and prosthetics tailored to the exact dimensions and anatomical features of the recipient. This is achieved by using biocompatible materials and cellular components to construct functional structures that seamlessly integrate with the patient’s body. For example, a patient requiring a hip replacement might receive a custom-designed implant perfectly matching their bone structure, leading to improved fit, reduced recovery time, and potentially better long-term outcomes. This personalized approach minimizes the risk of rejection and complications associated with off-the-shelf implants. The process often involves scanning the patient’s anatomy using imaging techniques like CT or MRI, then designing and 3D printing the implant based on the resulting data. The precision of 3D printing allows for intricate designs that are impossible to create using traditional manufacturing methods.
3D Printing in Tailored Drug Delivery Systems
3D printing offers remarkable possibilities for creating personalized drug delivery systems. These systems can be designed to release medication at specific rates and locations within the body, optimizing drug efficacy and minimizing side effects. For instance, a patient undergoing chemotherapy might benefit from a 3D-printed implant that slowly releases the drug over time, reducing the frequency of injections and improving patient comfort. Similarly, 3D-printed drug delivery systems can be tailored to release medication directly to a tumor site, increasing drug concentration at the target and reducing systemic toxicity. The ability to control the release kinetics and spatial distribution of the drug is a significant advantage over traditional methods.
3D-Printed Organoids for Personalized Drug Testing and Disease Modeling
3D-printed organoids, miniature three-dimensional tissue models, are emerging as powerful tools for personalized drug testing and disease modeling. These organoids can be created from a patient’s own cells, providing a highly accurate representation of their specific physiology and disease state. This allows researchers to test the efficacy and toxicity of drugs on a patient-specific model before administering them, significantly reducing the risk of adverse reactions and improving treatment outcomes. For example, a patient with a specific type of cancer could have a 3D-printed organoid created from their tumor cells. This organoid could then be used to screen different drugs, identifying the most effective treatment option with minimal side effects for that particular patient.
| Method | Advantages | Disadvantages | Applications |
|---|---|---|---|
| 3D-Printed Drug Delivery Systems | Precise drug release, targeted delivery, reduced side effects, personalized dosage, improved patient compliance | High initial cost, complex design and manufacturing, potential for biocompatibility issues, limited long-term stability in some cases | Cancer treatment, chronic disease management, ophthalmic drug delivery, localized pain relief |
| Traditional Drug Delivery Methods (e.g., oral, injection) | Relatively low cost, established manufacturing processes, widespread availability | Inconsistent drug levels, systemic side effects, poor patient compliance, limited targeting capabilities | Wide range of diseases and conditions |
Advancements in Biomaterials for 3D Printing
The ability to create functional tissues and organs hinges on the development of bioinks—the materials used in 3D bioprinting. These aren’t just any inks; they’re carefully engineered substances that need to be biocompatible, supporting cell growth and integration while also possessing the right mechanical properties to create stable, three-dimensional structures. The advancements in biomaterials are pushing the boundaries of what’s possible in regenerative medicine and beyond.
The quest for perfect bioinks is a fascinating blend of materials science and biology. Researchers are constantly exploring new materials and modifying existing ones to create bioinks that better mimic the natural extracellular matrix (ECM), the complex scaffold that supports cells in living tissues. This complex interplay between material properties and biological response is driving innovation in this field.
Biocompatible and Biodegradable Materials
The ideal bioink needs to be biocompatible, meaning it doesn’t trigger an adverse immune response or harm the cells it’s meant to support. Furthermore, biodegradability is often desirable; the material should gradually break down and be replaced by the patient’s own tissue as the printed construct integrates. Natural polymers like collagen, alginate, and hyaluronic acid are frequently used, offering good biocompatibility and tunable mechanical properties. Synthetic polymers, such as poly(lactic-co-glycolic acid) (PLGA) and polycaprolactone (PCL), provide additional advantages like controlled degradation rates and improved mechanical strength, although careful consideration of their potential toxicity is necessary. The ongoing research focuses on optimizing these materials and exploring new bio-derived or synthetic polymers to enhance biocompatibility, degradation profiles, and mechanical properties. For instance, researchers are exploring the use of decellularized extracellular matrices, which retain the structural complexity of native tissues while being immunologically inert.
Comparison of Bioinks Used in 3D Bioprinting
The choice of bioink significantly impacts the success of 3D bioprinting. Different bioinks offer unique advantages and disadvantages depending on the application.
- Hydrogels: Hydrogels are water-based polymers that form a gel-like structure. They are highly biocompatible and can easily incorporate cells, making them a popular choice for 3D bioprinting. However, their relatively low mechanical strength can be a limitation. Examples include alginate, collagen, and hyaluronic acid hydrogels.
- Cell-laden Inks: These inks directly incorporate cells within the bioink matrix. This allows for the creation of functional tissues with a pre-defined cellular organization. However, maintaining cell viability and uniform distribution within the ink during printing can be challenging. Many cell-laden inks utilize hydrogels as the base material, adding cells and potentially growth factors to promote tissue regeneration.
- Ceramic-based Bioinks: These bioinks offer superior mechanical strength compared to hydrogels. They are often used in applications requiring high structural integrity, such as bone tissue engineering. However, their biocompatibility needs careful consideration and optimization.
Challenges in Mimicking Native Tissue Complexity
Creating bioinks that truly mimic the complexity of native tissues remains a significant challenge. Native tissues possess intricate architectures, gradients of biochemical cues, and complex mechanical properties. Current bioinks often fall short in replicating this level of complexity. One major challenge is achieving the precise control over the microstructure and mechanical properties of the printed constructs to match the specific tissue being replicated. Another challenge lies in creating bioinks that can deliver multiple cell types and growth factors in a spatially controlled manner, mimicking the natural heterogeneity of tissues. Finally, integrating vascular networks within larger constructs to ensure adequate nutrient and oxygen supply is crucial but technically demanding. Overcoming these challenges requires further advancements in materials science, bioengineering, and 3D printing technologies.
3D Printing in Regenerative Medicine: The Future Of 3D Printing In Advancing Medical Research
Regenerative medicine, the field focused on repairing or replacing damaged tissues and organs, is experiencing a revolution thanks to 3D printing. This innovative technology offers unprecedented possibilities for creating intricate structures that mimic the complexity of human tissues, paving the way for personalized treatments and breakthroughs in healing. The ability to precisely control the architecture and composition of these printed constructs is key to their success in promoting tissue regeneration.
3D printing’s impact on regenerative medicine spans several crucial areas. It allows for the creation of scaffolds—temporary structures that provide support for cells to grow and regenerate—with highly customized designs tailored to the specific needs of each patient. Furthermore, 3D bioprinting, a more advanced technique, enables the direct deposition of cells alongside biomaterials, creating living tissues and organs with intricate vascular networks. This represents a significant step toward creating functional replacements for damaged or diseased tissues.
3D printing’s revolution in medical research is just getting started, paving the way for personalized prosthetics and intricate organ models. This rapid prototyping relies on lightning-fast data transfer, a need perfectly met by the advancements detailed in this article on How 5G Will Enable Breakthroughs in Autonomous Vehicles , because the same high-speed connectivity that fuels self-driving cars can similarly accelerate the complex data processing crucial for advanced 3D bioprinting.
Ultimately, this synergy will propel medical breakthroughs forward at an unprecedented pace.
3D-Printed Scaffolds for Tissue Regeneration
3D printing allows the creation of scaffolds with precisely controlled porosity, surface features, and mechanical properties. These scaffolds serve as a framework for cell attachment, proliferation, and differentiation, guiding the regeneration process. The material selection is crucial, with biodegradable polymers like polylactic acid (PLA) and polycaprolactone (PCL) being commonly used due to their biocompatibility and ability to degrade over time, leaving behind regenerated tissue. The design of the scaffold itself is also critical, mimicking the natural extracellular matrix (ECM) of the tissue being regenerated to optimize cell behavior. For example, a scaffold designed for bone regeneration might incorporate a porous structure to allow for vascularization and nutrient diffusion, while a scaffold for cartilage regeneration would need to possess a specific stiffness and flexibility to match the native tissue.
3D Bioprinting of Complex Tissues and Organs
3D bioprinting takes the technology a step further by incorporating living cells into the printing process. This allows for the creation of functional tissues and organs with complex architectures, including vascular networks crucial for nutrient and oxygen supply. The process involves the precise deposition of bioinks—mixtures of cells, biomaterials, and growth factors—layer by layer, creating a three-dimensional structure that closely resembles the target tissue. While still in its early stages, 3D bioprinting holds immense potential for creating functional liver tissues, skin grafts, and even entire organs, offering a revolutionary approach to organ transplantation and overcoming the limitations of donor organ availability. Researchers are actively exploring different bioinks and printing techniques to improve the viability and functionality of bioprinted tissues.
3D-Printed Bone Grafts and Cartilage Replacements
3D-printed bone grafts represent a significant advancement in orthopedic surgery. These grafts can be tailored to the precise shape and size of the bone defect, improving the fit and reducing the risk of complications.
Hypothetical 3D-Printed Bone Graft: Imagine a patient requiring a bone graft for a complex fracture in the tibia. A 3D-printed graft could be designed using computed tomography (CT) scan data to perfectly match the patient’s anatomy. The graft itself could be composed of a hydroxyapatite-reinforced polycaprolactone (PCL) composite. Hydroxyapatite mimics the mineral component of natural bone, providing structural support and promoting bone integration, while the PCL provides biodegradability and a scaffold for bone cell growth. The graft’s porous structure would allow for bone ingrowth and vascularization. During surgery, the 3D-printed graft would be precisely positioned and secured using appropriate fixation techniques. The porous structure facilitates bone cell infiltration and new bone formation, gradually replacing the printed scaffold over time.
Similarly, 3D printing is showing promise in creating cartilage replacements. Cartilage has limited self-repair capabilities, making it challenging to treat cartilage damage. 3D-printed cartilage constructs, often using materials like alginate or collagen hydrogels seeded with chondrocytes (cartilage cells), offer a potential solution for repairing damaged articular cartilage, alleviating pain and improving joint function. The precise control over the structure and composition of these constructs allows for the creation of grafts with the appropriate mechanical properties and biochemical cues to promote cartilage regeneration.
The Role of 3D Printing in Drug Discovery and Development
Source: thisvideorocks.com
3D printing, also known as additive manufacturing, is revolutionizing various fields, and its impact on drug discovery and development is particularly noteworthy. This technology offers unprecedented opportunities to accelerate the drug development process, personalize treatments, and ultimately improve patient outcomes. By enabling the creation of complex structures with intricate designs, 3D printing is transforming how we approach drug research and formulation.
3D printing accelerates drug discovery by enabling high-throughput screening of drug candidates. Traditional methods for testing drug efficacy involve laborious manual processes. 3D printing allows for the rapid prototyping of microfluidic devices and organ-on-a-chip models. These miniature, 3D-printed organs mimic the physiological functions of human organs, providing a more accurate and efficient platform for screening potential drug candidates. This high-throughput approach significantly reduces the time and cost associated with identifying promising drug leads. For example, researchers can print arrays of tiny chambers, each containing a different drug candidate and cell type, allowing them to simultaneously test hundreds or even thousands of compounds.
3D-Printed Models for Studying Drug Interactions and Pharmacokinetics
3D-printed models are invaluable tools for studying drug interactions and pharmacokinetics. Researchers can create patient-specific anatomical models, such as livers or tumors, to simulate drug absorption, distribution, metabolism, and excretion (ADME) processes. These models provide a more realistic representation of how a drug will behave in the body compared to traditional 2D cell cultures or animal models. For instance, a 3D-printed liver model can be used to assess how a new drug is metabolized, allowing researchers to predict potential drug-drug interactions and optimize dosage regimens. This approach is particularly crucial for personalized medicine, where treatment is tailored to an individual’s unique genetic makeup and physiological characteristics.
Personalized Drug Formulations Using 3D Printing
The potential of 3D printing in creating personalized drug formulations is immense. This technology allows for the precise control over drug release profiles, enabling the creation of customized dosage forms tailored to individual patient needs. For example, 3D printing can be used to create tablets with varying drug concentrations or to design implantable drug delivery devices that release medication at a specific rate over a prolonged period. This personalized approach can improve drug efficacy, reduce side effects, and enhance patient compliance.
A Hypothetical Experiment: 3D-Printed Drug Delivery Systems for Improved Drug Efficacy
Let’s consider a hypothetical experiment using 3D-printed drug delivery systems to improve the efficacy of a cancer drug. The drug, hypothetical drug X, is known to have poor bioavailability and short half-life, limiting its effectiveness. The experiment involves designing and 3D-printing a biodegradable, porous scaffold loaded with drug X. The scaffold is designed to mimic the tumor microenvironment, providing a sustained release of the drug directly to the tumor site. The 3D-printed scaffold’s porosity and biodegradability are optimized to ensure controlled drug release over several weeks, minimizing systemic exposure and maximizing drug concentration at the tumor. The experiment compares the efficacy of the 3D-printed drug delivery system against traditional intravenous administration of drug X in a preclinical animal model. The primary outcome measures are tumor growth inhibition, drug concentration in tumor tissue, and systemic toxicity. This hypothetical experiment demonstrates how 3D printing can be utilized to overcome limitations of traditional drug delivery methods and improve therapeutic outcomes.
Challenges and Future Directions of 3D Printing in Medical Research
The rapid advancements in 3D printing technology hold immense promise for revolutionizing medical research, but several significant hurdles remain before widespread adoption becomes a reality. Overcoming these challenges will require collaborative efforts from researchers, engineers, regulators, and ethicists to unlock the full potential of this transformative technology in healthcare. This section delves into the key obstacles and potential pathways forward.
Major Challenges Hindering Widespread Adoption
Several factors currently limit the widespread use of 3D printing in medical research. These range from technical limitations to regulatory and ethical concerns. Addressing these challenges is crucial for realizing the full potential of this technology.
- Cost and Scalability: The high initial investment in 3D bioprinters and bioinks, coupled with the often-complex and time-consuming printing processes, makes it a costly endeavor. Scaling up production to meet the demands of large-scale clinical trials remains a significant challenge. For example, the cost of producing a single complex organoid using current technology can be prohibitive for widespread research use.
- Material Limitations: The range of biocompatible and bio-functional materials suitable for 3D bioprinting is still limited. Developing materials that accurately mimic the complex properties of native tissues, while being easily printable and readily available, is an ongoing area of active research. For instance, creating a bioink that perfectly replicates the intricate extracellular matrix of a human heart remains a significant challenge.
- Resolution and Accuracy: Achieving high-resolution and accurate printing of complex three-dimensional structures is essential for creating functional tissues and organs. Current technologies often struggle to create the intricate vascular networks and cellular arrangements necessary for tissue viability and function. Improvements in printing resolution and precision are vital for advancing the field.
The Need for Improved Resolution and Accuracy in 3D Bioprinting
The precision of 3D bioprinting directly impacts the functionality and viability of the printed constructs. Current limitations in resolution result in inconsistencies in cell distribution, insufficient vascularization, and compromised tissue architecture. This can lead to inadequate nutrient and oxygen supply, hindering cell survival and tissue integration. Advancements in printing techniques, such as microfluidic-based bioprinting or two-photon polymerization, offer potential solutions for achieving higher resolution and improved accuracy, enabling the creation of more complex and functional tissues. For example, the development of higher-resolution printers allows for the creation of more intricate vascular networks within engineered tissues, dramatically improving their viability and potential for transplantation.
Regulatory Hurdles and Ethical Considerations
The introduction of 3D-printed medical devices and tissues raises complex regulatory and ethical questions. The unique nature of these products requires a carefully considered regulatory framework to ensure safety and efficacy while fostering innovation.
Proposed Regulatory Framework for 3D-Printed Medical Products
A robust regulatory framework should address several key aspects: a standardized pre-clinical testing protocol to evaluate the safety and biocompatibility of 3D-printed materials; clear guidelines for clinical trials involving 3D-printed implants or tissues; a system for post-market surveillance to monitor the long-term performance and safety of these products; and mechanisms for addressing intellectual property rights and ensuring equitable access to these technologies. This framework should be flexible enough to adapt to the rapid advancements in the field while maintaining high standards of patient safety and ethical considerations. This would involve collaboration between regulatory bodies (like the FDA in the US and the EMA in Europe), researchers, manufacturers, and patient advocacy groups to establish clear guidelines and standards for 3D-printed medical products. The framework should balance the need for rigorous safety assessment with the need to encourage innovation and avoid stifling the development of potentially life-saving technologies.
Closure
The future of medicine is undeniably intertwined with the advancements in 3D printing. While challenges remain, the potential benefits – personalized treatments, accelerated drug discovery, and regenerative medicine breakthroughs – are too significant to ignore. As research continues and regulatory frameworks evolve, we can expect 3D printing to play an increasingly crucial role in shaping a healthier future for all. The possibilities are as vast as our imaginations, and the journey is only just beginning.
