How Smart Sensors are Changing the Healthcare Landscape: Forget clunky machines and invasive procedures. We’re diving into the world of tiny, powerful sensors revolutionizing everything from diagnosis to treatment. Think personalized medicine delivered right to your wrist, early disease detection before you even notice symptoms, and surgeries guided with unprecedented precision. It’s a tech revolution happening now, and it’s changing lives.
This miniaturization and increased processing power aren’t just incremental improvements; they’re game-changers. Smart sensors are enabling remote patient monitoring, allowing doctors to track vital signs and intervene proactively. They’re personalizing treatments based on individual genetic profiles and real-time physiological data. And they’re even paving the way for revolutionary advancements like bio-integrated sensors and nanotechnology in medicine.
The Rise of Smart Sensors in Healthcare
The healthcare industry is undergoing a dramatic transformation, fueled by the rapid advancement of smart sensor technology. From simple thermometers to sophisticated wearable devices, sensors are revolutionizing how we diagnose, treat, and monitor health conditions. This evolution isn’t just about adding more gadgets; it’s about creating a more proactive, personalized, and efficient healthcare system. The integration of smart sensors represents a significant leap forward, offering unprecedented levels of data collection and analysis, leading to improved patient outcomes and reduced healthcare costs.
This progress is largely due to the convergence of several technological advancements. Initially, sensors were bulky, expensive, and limited in their capabilities. However, the miniaturization of electronics and the exponential increase in processing power have dramatically improved the performance and affordability of smart sensors. This has allowed for the development of smaller, more energy-efficient devices capable of collecting a wider range of physiological data with greater accuracy. This miniaturization also enables the creation of less invasive and more comfortable devices for patients.
Key Features and Functionalities of Smart Sensors in Medical Applications
Smart sensors employed in healthcare are not simply measurement tools; they are intelligent systems capable of data processing and communication. These features are crucial for their effectiveness. They go beyond simple data acquisition, incorporating sophisticated algorithms for data analysis and interpretation. This allows for real-time monitoring, early detection of anomalies, and automated alerts to healthcare providers. Furthermore, many smart sensors are wireless, enabling remote monitoring and reducing the need for frequent hospital visits.
Impact of Miniaturization and Improved Processing Power
The impact of miniaturization and increased processing power on smart sensors is profound. Consider implantable sensors: earlier versions were large and required significant surgical procedures. Modern advancements allow for smaller, less invasive implants, such as glucose sensors for diabetes management, which are significantly less disruptive to patients’ lives. The improved processing power allows these miniaturized sensors to perform complex calculations on the collected data, identifying patterns and trends that might otherwise be missed. For example, a smart patch monitoring heart rate variability can not only record the data but also analyze it to detect early signs of cardiac arrhythmias, alerting the patient and their physician. This proactive approach is a game-changer in preventative healthcare.
Smart Sensors in Diagnostics and Monitoring: How Smart Sensors Are Changing The Healthcare Landscape
Source: mdpi.com
Smart sensors are revolutionizing healthcare diagnostics and monitoring, moving beyond traditional methods to offer faster, more accurate, and often less invasive ways to assess health. This shift is driven by miniaturization, improved sensor technology, and the rise of powerful data analytics. The ability to continuously monitor vital signs and detect subtle changes opens doors to earlier disease detection and more personalized treatment plans.
Early Disease Detection with Smart Sensors
Early detection is crucial for improving patient outcomes in many diseases. Smart sensors are playing a vital role in this area. For example, wearable sensors embedded in smartwatches or fitness trackers can continuously monitor heart rate variability, providing early warnings of potential cardiac issues. Similarly, sensors in smart scales can detect subtle changes in weight, a potential indicator of fluid retention or other health problems. Continuous glucose monitors (CGMs) for diabetics provide real-time glucose readings, preventing severe hypoglycemic or hyperglycemic episodes. These are just a few examples of how smart sensors are enabling proactive health management. The detection of subtle changes, often missed by traditional periodic check-ups, allows for timely interventions and improved patient outcomes.
Accuracy and Efficiency: Smart Sensors vs. Traditional Methods
Smart sensors offer several advantages over traditional diagnostic methods. Traditional methods, such as blood tests or X-rays, often require a visit to a clinic or hospital, involve a time delay for results, and can be invasive. Smart sensors, on the other hand, can provide continuous, real-time data, often non-invasively. While the accuracy of smart sensors varies depending on the type and application, many studies show comparable or even superior accuracy in specific areas compared to traditional methods. For instance, some studies have demonstrated that continuous glucose monitoring via CGM provides more accurate reflection of glucose fluctuations than traditional finger-prick methods. However, it’s crucial to acknowledge that smart sensors are not a replacement for traditional methods in all cases; they are often complementary tools, enhancing the accuracy and efficiency of overall diagnosis. For example, a smart sensor might flag a potential issue, prompting a follow-up with traditional diagnostic tests for confirmation.
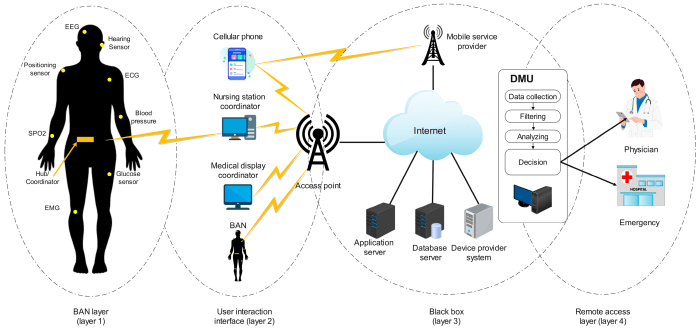
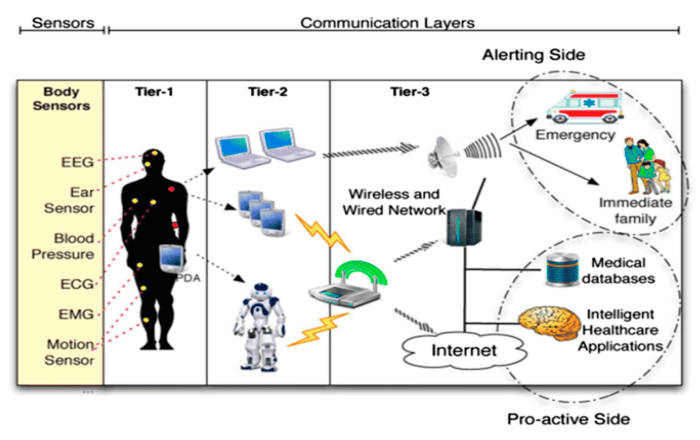
Remote Patient Monitoring and Telehealth
Smart sensors are a cornerstone of remote patient monitoring (RPM) and telehealth. RPM allows healthcare providers to monitor patients remotely, reducing the need for frequent in-person visits. This is particularly beneficial for patients with chronic conditions or those living in remote areas. Implantable sensors, wearable sensors, and even home-based sensors transmit data wirelessly to healthcare providers, enabling continuous monitoring of vital signs such as heart rate, blood pressure, and oxygen saturation. This real-time data facilitates timely interventions, reducing hospital readmissions and improving overall patient outcomes. The convenience and cost-effectiveness of RPM are also significant benefits for both patients and healthcare systems. For example, patients with congestive heart failure can be monitored for early signs of decompensation, allowing for proactive adjustments to medication or treatment.
Types of Smart Sensors in Diagnostics
Smart sensors come in various forms, each with its own strengths and weaknesses. The following table summarizes some key types:
| Sensor Type | Application | Advantages | Disadvantages |
|---|---|---|---|
| Wearable Sensors (e.g., smartwatches, fitness trackers) | Heart rate, activity level, sleep patterns, ECG, SpO2 | Continuous monitoring, convenience, affordability (for some types) | Accuracy can vary, susceptible to interference, data privacy concerns |
| Implantable Sensors (e.g., pacemakers, insulin pumps) | Heart rhythm, glucose levels, intracranial pressure | Continuous, accurate data, direct measurement | Surgical implantation required, potential for complications, higher cost |
| Lab-on-a-Chip Devices (microfluidic devices) | Blood analysis, DNA sequencing, point-of-care diagnostics | Rapid results, small sample size, portability, automation potential | High initial cost, requires specialized training for operation |
Smart Sensors in Treatment and Therapy
Smart sensors are revolutionizing healthcare beyond diagnostics and monitoring; they’re actively shaping treatment and therapy, leading to more precise, personalized, and effective interventions. This shift is driven by the ability of these miniature devices to collect real-time data, enabling continuous monitoring and adaptive adjustments to treatment plans. The integration of smart sensors is transforming drug delivery, personalizing medicine, and enhancing surgical precision.
Smart Sensors in Drug Delivery Systems
Smart sensors are integral to the development of advanced drug delivery systems, moving beyond simple timed-release mechanisms. These systems utilize sensors to monitor various physiological parameters, such as blood glucose levels, medication concentration in the bloodstream, or even the presence of specific biomarkers. This data allows for dynamic adjustments to drug release, optimizing therapeutic efficacy and minimizing side effects. For instance, an implantable insulin pump equipped with a glucose sensor can automatically adjust insulin delivery based on real-time blood glucose readings, eliminating the need for manual adjustments and improving glycemic control in diabetes management. This represents a significant leap forward from traditional methods, offering personalized and responsive treatment.
Smart Sensors in Personalized Medicine and Targeted Therapies
The promise of personalized medicine hinges on the ability to tailor treatments to individual patients based on their unique genetic makeup, lifestyle, and disease characteristics. Smart sensors play a crucial role in this paradigm shift. By continuously monitoring a patient’s response to therapy, these sensors provide valuable data that allows clinicians to fine-tune treatment plans in real-time. For example, sensors embedded in a medication patch could track drug absorption and monitor patient compliance, enabling adjustments to dosage or medication type based on individual needs. This personalized approach can improve treatment outcomes, reduce adverse effects, and optimize therapeutic efficacy. Consider cancer treatment: sensors monitoring tumor response to chemotherapy can inform adjustments to the treatment regimen, maximizing effectiveness while minimizing harmful side effects.
Smart Sensors in Improving Surgical Procedures
Smart sensors are enhancing the precision and safety of surgical procedures. Intraoperative sensors provide surgeons with real-time feedback on vital signs, tissue properties, and the effectiveness of surgical interventions. For example, sensors integrated into surgical instruments can provide information about tissue temperature, pressure, and force, allowing surgeons to perform delicate procedures with greater precision and minimizing the risk of tissue damage. Robotic surgery, increasingly reliant on smart sensors, provides surgeons with enhanced dexterity and visualization, leading to smaller incisions, reduced trauma, and faster recovery times. Imagine a scenario where a sensor embedded in a surgical tool provides real-time feedback on the amount of bleeding during a procedure, allowing for immediate intervention and preventing excessive blood loss.
Smart Sensor Integration in a Prosthetic Limb
Imagine a prosthetic limb equipped with a network of smart sensors. These sensors would continuously monitor muscle activity, limb position, and environmental factors. Pressure sensors in the socket would detect the level of force applied, ensuring a comfortable and secure fit. Flex sensors integrated into the artificial joints would mimic the natural range of motion, allowing for fluid and intuitive movement. Furthermore, haptic sensors could provide feedback to the user, simulating the sensation of touch. This sophisticated prosthetic would not only restore mobility but also improve the quality of life for amputees by providing a more natural and responsive experience. This system could learn and adapt to the user’s individual movements and preferences over time, becoming increasingly personalized and effective.
Data Management and Analysis with Smart Sensors
Source: mdpi.com
Smart sensors are revolutionizing healthcare, offering real-time patient monitoring and predictive diagnostics. This data-driven approach mirrors the potential of AI in tackling global food insecurity; check out this insightful piece on how AI can help solve this critical issue: How AI Can Help Solve Global Hunger and Food Insecurity. Similarly, the precision and efficiency offered by smart sensors promise a future of proactive, personalized healthcare.
The explosion of data generated by smart sensors in healthcare presents both incredible opportunities and significant challenges. Effectively managing and analyzing this data is crucial for realizing the full potential of this technology, leading to improved patient outcomes and more efficient healthcare systems. This requires robust infrastructure, sophisticated analytical techniques, and a strong commitment to data privacy and ethical considerations.
The sheer volume, velocity, and variety of data from smart sensors demand innovative approaches to data management. We’re talking terabytes, if not petabytes, of information streaming in from wearable devices, implantable sensors, and environmental monitors. This data needs to be stored securely, accessed efficiently, and integrated with existing Electronic Health Records (EHR) systems for a comprehensive patient view.
Secure Data Storage and Management
Several methods are employed to securely store and manage the vast amounts of data generated by smart sensors. Cloud-based solutions offer scalability and accessibility, but require robust security measures like encryption at rest and in transit, access control lists, and regular security audits. On-premise solutions offer greater control over data but demand significant investment in infrastructure and maintenance. Hybrid approaches, combining cloud and on-premise storage, offer a balance between scalability and control. Regardless of the chosen method, data anonymization and de-identification techniques are vital to protect patient privacy. For instance, data might be aggregated to show trends without revealing individual patient information. Furthermore, blockchain technology is emerging as a potential solution for enhancing data security and integrity through its decentralized and immutable nature.
The Role of Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are indispensable tools for extracting meaningful insights from the massive datasets generated by smart sensors. ML algorithms can identify patterns and correlations that would be impossible for humans to detect manually. For example, ML models can analyze data from wearable sensors to predict the onset of a heart attack or identify subtle changes indicating the progression of a chronic disease. AI-powered diagnostic tools can analyze medical images with greater speed and accuracy than human experts, leading to earlier and more precise diagnoses. Predictive analytics, leveraging AI and ML, can optimize treatment plans, personalize medicine, and improve resource allocation within healthcare systems. For instance, an AI system could predict patient readmission rates based on sensor data and adjust discharge plans accordingly.
Data Privacy and Security Challenges
The use of smart sensors in healthcare raises significant data privacy and security concerns. The sensitive nature of patient health data makes it a prime target for cyberattacks. Challenges include ensuring data integrity, preventing unauthorized access, and complying with data protection regulations such as HIPAA and GDPR. Data breaches can have devastating consequences, leading to identity theft, financial losses, and reputational damage. Therefore, robust cybersecurity measures, including encryption, access controls, intrusion detection systems, and regular security audits, are essential. Furthermore, the development and implementation of clear data governance policies and procedures are critical to ensure responsible data handling.
Ethical Considerations Surrounding Patient Data
Ethical considerations are paramount in the use of patient data from smart sensors. Issues such as informed consent, data ownership, and the potential for bias in algorithms need careful consideration. Patients must be fully informed about how their data will be collected, used, and protected. Clear and transparent policies are needed to address data ownership and access rights. Moreover, algorithms used to analyze sensor data must be rigorously tested to ensure fairness and avoid perpetuating existing health disparities. For example, an algorithm trained on data from a predominantly white population might not perform as well for patients from other ethnic backgrounds, leading to biased diagnoses or treatment recommendations. Ongoing monitoring and evaluation are necessary to identify and mitigate potential ethical risks.
The Future of Smart Sensors in Healthcare
The integration of smart sensors in healthcare is still in its nascent stages, yet the potential for revolutionizing patient care, diagnostics, and treatment is undeniable. We’re on the cusp of a healthcare transformation driven by increasingly sophisticated sensor technologies, paving the way for personalized medicine and proactive healthcare management. The next decade promises to be particularly exciting as we witness the convergence of miniaturization, artificial intelligence, and advanced materials science to create truly transformative medical devices.
Potential Future Applications of Smart Sensors
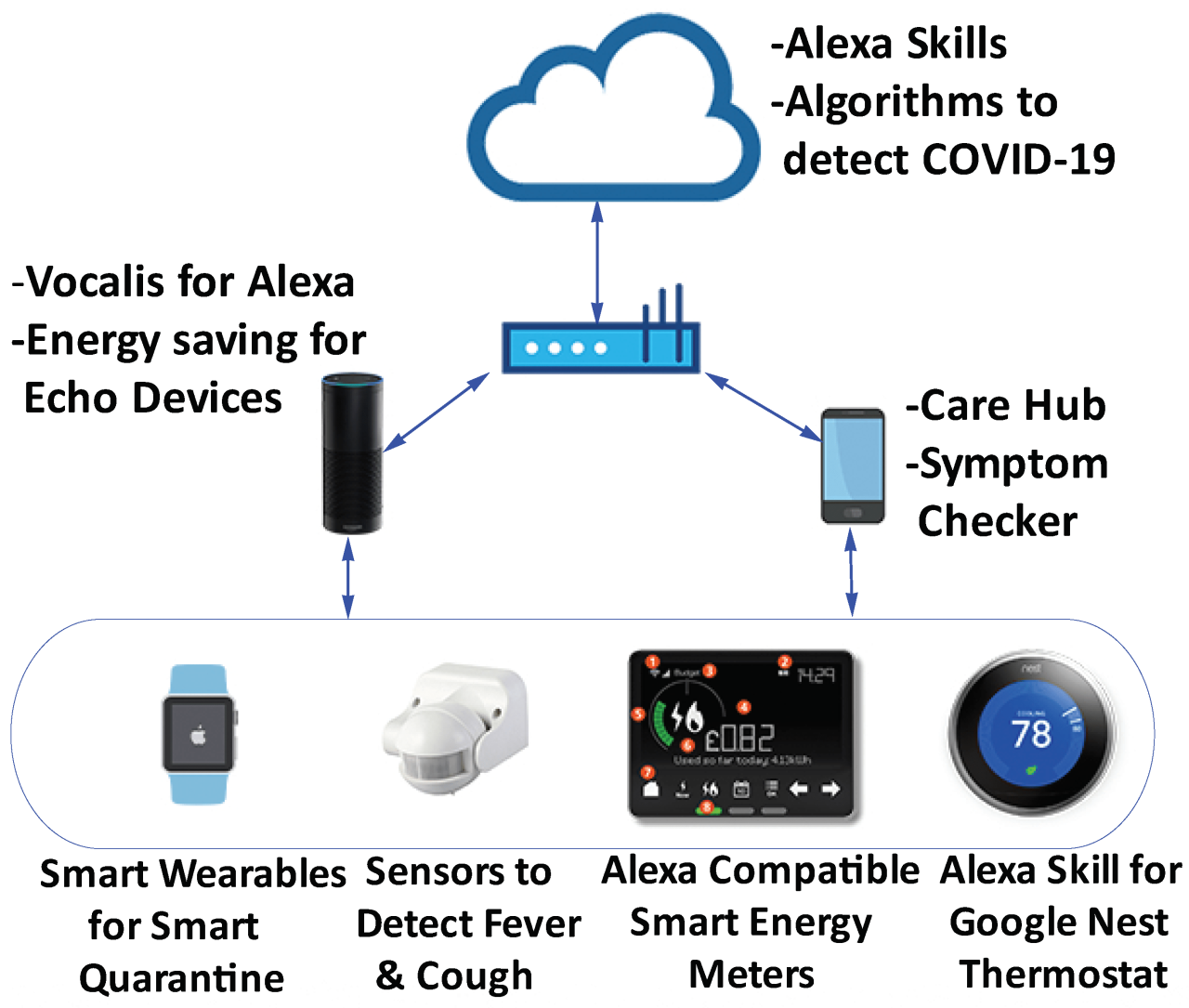
Smart sensors are poised to expand their reach far beyond current applications. Imagine implantable sensors that continuously monitor vital signs, alerting medical professionals to potential problems before they become critical. Wearable devices could become even more sophisticated, providing detailed analysis of physical activity, sleep patterns, and even emotional states, offering personalized insights into overall well-being. Beyond individual monitoring, smart sensors could play a crucial role in public health initiatives, tracking the spread of infectious diseases in real-time and enabling rapid responses to outbreaks. For instance, a network of environmental sensors could detect the presence of airborne pathogens, triggering early warnings and preventative measures.
The Impact of Nanotechnology and Bio-integrated Sensors
Nanotechnology promises to shrink sensors to microscopic sizes, enabling minimally invasive procedures and continuous monitoring without the discomfort or limitations of larger devices. Bio-integrated sensors, seamlessly incorporated into the body, could provide continuous, real-time data on a wide range of physiological parameters. These advancements could lead to earlier detection of diseases like cancer, enabling more effective treatments and improved patient outcomes. For example, nanosensors could be injected into the bloodstream to detect circulating tumor cells, providing an early warning sign of cancer development. Furthermore, biocompatible materials are being developed to ensure long-term integration and minimize the risk of adverse reactions.
Technological Advancements Needed to Overcome Current Limitations
Despite the impressive progress, several challenges remain. One major hurdle is the development of more energy-efficient sensors, capable of operating for extended periods without requiring frequent battery replacements or recharging. Another critical area is data security and privacy. The vast amounts of sensitive patient data generated by smart sensors require robust security measures to prevent breaches and protect patient confidentiality. Finally, the integration of data from multiple sensors into a unified, easily interpretable format is a significant technological challenge. Standardization of data formats and the development of advanced data analytics tools are crucial to unlock the full potential of smart sensor technology.
Potential Breakthroughs in Smart Sensor Technology (Next 5-10 Years)
The next 5-10 years will likely witness significant advancements in smart sensor technology. These advancements are likely to be driven by both incremental improvements and fundamental breakthroughs.
Several key areas are ripe for significant progress:
- Improved Biocompatibility and Integration: Development of sensors that seamlessly integrate with the body, minimizing immune response and ensuring long-term functionality.
- Wireless Power Transfer: Eliminating the need for battery replacements through efficient wireless power transfer technologies, enabling truly implantable devices.
- Advanced Data Analytics: Development of sophisticated algorithms for analyzing the vast amounts of data generated by smart sensors, leading to more accurate diagnoses and personalized treatment plans. For example, AI-powered diagnostic tools that analyze sensor data to detect subtle changes indicative of disease onset.
- Miniaturization and Increased Sensitivity: Creating even smaller and more sensitive sensors capable of detecting minute changes in physiological parameters, leading to earlier and more accurate diagnoses.
- Enhanced Security and Privacy: Implementation of robust security protocols and encryption techniques to protect the sensitive patient data collected by smart sensors.
Illustrative Example: Continuous Glucose Monitoring
Source: mdpi-res.com
Smart sensors are revolutionizing diabetes management, and continuous glucose monitoring (CGM) systems stand as a prime example. These systems offer a significant leap forward from traditional finger-prick blood glucose testing, providing real-time data and empowering individuals with diabetes to make informed decisions about their health.
CGM systems typically consist of a small sensor inserted just beneath the skin, usually in the abdomen. This sensor contains a tiny glucose sensor that measures interstitial fluid glucose levels. The sensor transmits this data wirelessly to a receiver, often a smartphone or dedicated device, providing a continuous stream of glucose readings. This constant monitoring allows users to track glucose fluctuations throughout the day and night, gaining a much clearer picture of their metabolic activity than ever before.
Sensor Design and Functionality
The sensor itself is a marvel of miniaturization. It’s designed to be biocompatible, minimizing the risk of irritation or rejection by the body. The glucose sensor utilizes electrochemical techniques, often employing an enzyme-based reaction to measure glucose concentration. The data is then processed by a microchip within the sensor, which digitally encodes the information for wireless transmission. This transmission typically uses Bluetooth technology to communicate with the receiver device, providing near real-time updates to the user. The sensor’s battery life varies depending on the specific model but generally lasts for several days before needing replacement.
Impact on Patient Care, How Smart Sensors are Changing the Healthcare Landscape
The impact of CGM systems on patient care is substantial. By providing continuous glucose data, these systems allow for proactive management of blood sugar levels, reducing the risk of both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). This leads to better glycemic control, which in turn reduces the long-term complications associated with diabetes, such as heart disease, kidney disease, and nerve damage. Furthermore, CGM data empowers individuals with diabetes to make more informed decisions about their diet, exercise, and insulin administration, promoting a greater sense of control and autonomy over their condition. The data generated by CGM systems also benefits healthcare providers, allowing them to monitor patients remotely and make adjustments to treatment plans as needed. For example, a sudden drop in glucose levels can trigger an alert, enabling timely intervention and preventing potentially dangerous hypoglycemic episodes. The data also provides valuable insights for research, contributing to a deeper understanding of diabetes and the development of more effective treatments.
Closing Notes
The integration of smart sensors in healthcare isn’t just a technological advancement; it’s a fundamental shift in how we approach health and wellness. From early detection and personalized treatment to improved surgical precision and remote patient monitoring, the potential is limitless. While challenges remain in data security and ethical considerations, the future of healthcare is undeniably intertwined with the continued innovation and responsible implementation of this transformative technology. Get ready for a healthier, smarter tomorrow, powered by the tiniest of tech marvels.
