How Big Data is Shaping the Future of Healthcare? It’s not just buzzwords; it’s a revolution. Imagine a world where diseases are diagnosed faster, treatments are personalized, and healthcare is more accessible than ever before. That’s the promise of big data, and it’s already unfolding. From predicting outbreaks to optimizing hospital resources, the sheer volume of patient information is transforming how we approach health and wellness. This isn’t just about numbers; it’s about lives.
We’re diving deep into how this data deluge is impacting everything from disease detection and personalized medicine to streamlining hospital operations and even tackling health disparities. Get ready to see how the future of healthcare is being written, one data point at a time.
Improved Diagnostics and Treatment
Big data is revolutionizing healthcare, offering unprecedented opportunities to improve diagnostics, personalize treatments, and enhance public health management. The sheer volume, velocity, and variety of data generated – from patient records to genomic sequencing – are providing powerful insights previously unimaginable. This allows for more accurate and timely diagnoses, leading to better patient outcomes and a more efficient healthcare system.
Enhanced Diagnostic Accuracy and Speed
Big data analytics significantly accelerates and improves the accuracy of disease diagnosis. By analyzing massive datasets encompassing patient history, medical images, genetic information, and lifestyle factors, algorithms can identify patterns and anomalies indicative of specific diseases far more efficiently than traditional methods. For instance, AI-powered image analysis can detect subtle signs of cancer in medical scans, often earlier than human experts, leading to earlier intervention and improved survival rates. This speed and accuracy are particularly crucial in time-sensitive conditions like strokes or heart attacks.
Personalized Treatment Plans Through Machine Learning
Machine learning algorithms play a pivotal role in tailoring treatment plans to individual patient needs. By analyzing a patient’s unique characteristics – genetic makeup, medical history, lifestyle, and response to previous treatments – these algorithms can predict the likelihood of treatment success and identify potential adverse effects. This personalized approach allows doctors to select the most effective therapies while minimizing risks, leading to improved outcomes and reduced healthcare costs. For example, algorithms can predict which patients are most likely to respond to a particular cancer drug, allowing for targeted therapy and avoiding unnecessary side effects for those who wouldn’t benefit.
Predicting Disease Outbreaks and Managing Public Health Crises
Big data analytics is instrumental in predicting and managing public health crises. By analyzing data from various sources – social media, weather patterns, disease surveillance systems – algorithms can identify potential outbreaks early on, allowing for timely interventions to prevent widespread epidemics. For example, during the COVID-19 pandemic, analysis of mobility data and social media posts helped predict infection hotspots and inform public health strategies. Similarly, tracking the spread of influenza through data from doctor’s visits and hospital admissions allows for better resource allocation and targeted public health campaigns.
Impact on Drug Discovery and Development
Big data is significantly accelerating drug discovery and development. It facilitates target identification by analyzing genomic data to pinpoint specific genes or proteins involved in disease processes. This allows researchers to develop drugs that precisely target these mechanisms, leading to more effective and safer medications. Furthermore, big data is used to optimize clinical trials by identifying suitable patient populations, predicting trial outcomes, and accelerating the drug approval process. For example, analyzing patient data from previous trials can help predict which patients are most likely to respond to a new drug, reducing the size and cost of clinical trials.
Comparison of Traditional and Big Data-Driven Diagnostic Methods
| Feature | Traditional Methods | Big Data-Driven Approaches |
|---|---|---|
| Speed | Relatively slow, often involving manual analysis | Rapid, automated analysis of large datasets |
| Accuracy | Subject to human error and limitations of individual expertise | Potentially higher accuracy due to analysis of vast amounts of data and identification of subtle patterns |
| Cost | Can be expensive, especially for specialized tests | Initial investment in infrastructure and expertise required, but can lead to cost savings in the long run due to improved efficiency and reduced errors |
| Personalization | Limited personalization; treatment based on general guidelines | Highly personalized treatments tailored to individual patient characteristics |
Enhanced Patient Care and Monitoring
Big data is revolutionizing patient care, moving beyond reactive treatment to proactive, personalized health management. The ability to collect, analyze, and interpret massive datasets allows for a more comprehensive understanding of individual patient needs and the development of strategies to improve outcomes and enhance the overall patient experience. This shift towards preventative and personalized care is largely driven by advancements in wearable technology and remote monitoring capabilities.
The integration of big data into healthcare enables a more holistic approach to patient care, going beyond traditional clinic visits to encompass continuous monitoring and personalized interventions. This leads to improved treatment adherence, earlier detection of potential problems, and ultimately, better health outcomes.
Real-time Patient Data Collection via Wearable Sensors and Connected Devices
Wearable sensors, such as smartwatches and fitness trackers, coupled with connected medical devices like insulin pumps and blood pressure monitors, continuously collect a wealth of patient data. This data, ranging from heart rate and activity levels to blood glucose and sleep patterns, provides a detailed picture of a patient’s health status in real-time. This constant stream of information allows healthcare providers to identify potential issues early, adjust treatment plans proactively, and intervene before minor problems escalate into major health crises. For instance, a smartwatch detecting an irregular heartbeat could trigger an alert, allowing for immediate medical attention and potentially preventing a serious cardiac event. Similarly, continuous glucose monitoring systems can help diabetics manage their blood sugar levels effectively, reducing the risk of complications.
Remote Patient Monitoring and Improved Care Coordination
Big data significantly enhances remote patient monitoring (RPM) capabilities. Data collected from wearable sensors and connected devices is transmitted to secure cloud platforms, where it’s analyzed using sophisticated algorithms. This allows healthcare providers to monitor patients remotely, identify trends, and intervene as needed, even without in-person visits. This is particularly beneficial for patients with chronic conditions who require frequent monitoring or those living in remote areas with limited access to healthcare. Effective RPM reduces hospital readmissions, improves patient adherence to treatment plans, and enhances the overall efficiency of healthcare delivery. For example, a patient recovering from heart surgery can be monitored remotely for irregular heart rhythms or other complications, allowing for prompt intervention if needed.
Identifying High-Risk Patients
Big data analytics enables the identification of patients at high risk of readmission or adverse events. By analyzing historical data, including medical records, lab results, and lifestyle factors, algorithms can identify patterns and risk factors that predict potential complications. This allows healthcare providers to proactively intervene and implement preventative measures, reducing the likelihood of negative outcomes. For example, a predictive model might identify patients at high risk of developing pneumonia post-surgery, allowing for preventative measures such as early antibiotic treatment or closer monitoring. This proactive approach significantly improves patient safety and reduces healthcare costs associated with readmissions and complications.
Personalized Patient Education and Engagement
Big data can be leveraged to create personalized patient education and engagement strategies. By analyzing patient data and preferences, healthcare providers can tailor educational materials and communication methods to resonate with individual needs and learning styles. This approach enhances patient understanding of their condition, promotes treatment adherence, and improves overall health outcomes. For instance, a system could automatically generate personalized educational videos or interactive modules based on a patient’s specific condition, age, and learning preferences. This personalized approach fosters better patient engagement and improves the effectiveness of health education initiatives.
Ethical Considerations Regarding Patient Data Privacy and Security
The use of big data in healthcare raises several ethical considerations, particularly regarding the privacy and security of patient data. It is crucial to implement robust data protection measures to ensure patient confidentiality and prevent unauthorized access or misuse of sensitive information.
- Data Security: Implementing strong encryption, access controls, and regular security audits to protect patient data from breaches and unauthorized access.
- Data Privacy: Adhering to strict data privacy regulations, such as HIPAA (in the US) and GDPR (in Europe), and obtaining informed consent from patients before collecting and using their data.
- Data Anonymization and De-identification: Employing techniques to remove or mask identifying information from patient data while preserving its analytical value.
- Transparency and Accountability: Ensuring transparency in data collection and usage practices, and establishing mechanisms for accountability in case of data breaches or misuse.
- Algorithmic Bias: Addressing potential biases in algorithms used to analyze patient data to prevent discrimination and ensure equitable healthcare access.
Optimizing Healthcare Operations and Resource Allocation
Big data is revolutionizing healthcare, not just in improving patient outcomes, but also in streamlining operations and making the most of limited resources. By analyzing vast amounts of data, healthcare organizations can identify inefficiencies, predict future needs, and ultimately, deliver better care while reducing costs. This translates to a more sustainable and effective healthcare system for everyone.
The ability to analyze patient data, operational data, and even external factors like weather patterns allows for a level of predictive modeling previously unimaginable. This data-driven approach helps optimize resource allocation, leading to significant improvements in efficiency and cost reduction. For instance, hospitals can better predict patient volume, adjust staffing levels accordingly, and minimize wait times, leading to improved patient satisfaction and reduced operational expenses.
Predictive Modeling for Staffing and Resource Allocation
Predictive modeling uses historical data, current trends, and algorithms to forecast future needs. In healthcare, this is particularly useful for optimizing staffing levels. By analyzing past patient admissions, length of stay, and predicted demand based on factors like seasonal illnesses or public health events, hospitals can more accurately predict staffing requirements. This minimizes the risk of overstaffing (leading to unnecessary labor costs) or understaffing (resulting in compromised patient care and potential burnout among existing staff). For example, a hospital might use predictive modeling to anticipate a surge in emergency room visits during flu season, proactively scheduling additional nurses and doctors to handle the increased workload. This proactive approach ensures optimal patient care while managing costs effectively.
Big Data’s Role in Hospital Capacity Management and Patient Flow, How Big Data is Shaping the Future of Healthcare
Effective management of hospital capacity is crucial for efficient patient flow and overall operational efficiency. Big data allows for real-time monitoring of bed occupancy, operating room schedules, and patient throughput. This data provides a holistic view of hospital capacity, allowing administrators to identify bottlenecks and optimize resource allocation. For example, analyzing data on average length of stay for different procedures can help hospitals anticipate discharge times and plan for bed availability. Similarly, analyzing data on wait times in the emergency room can highlight areas for improvement, such as streamlining admission processes or optimizing triage procedures. This data-driven approach minimizes delays, improves patient flow, and enhances overall operational efficiency.
Data Integration and Interoperability in Healthcare
Integrating data from various sources – electronic health records (EHRs), medical devices, billing systems, and even external sources like public health databases – is crucial for leveraging the full potential of big data in healthcare. However, achieving interoperability, or the seamless exchange of data between different systems, remains a significant challenge. Different approaches exist, including the use of standardized data formats (like HL7 FHIR), cloud-based platforms for data sharing, and the development of interoperable healthcare information exchanges (HIEs). While challenges remain, the benefits of improved data integration and interoperability are undeniable, paving the way for more efficient and effective healthcare delivery. The key difference between these approaches often lies in the level of standardization, the security measures implemented, and the cost of implementation. A well-designed HIE, for example, may be more expensive to implement initially but offers a more comprehensive and secure solution compared to a simpler, less standardized approach.
Visual Representation of Big Data Streamlining Healthcare Workflows
Imagine a dynamic dashboard displaying real-time information. One section shows current bed occupancy in different wards, color-coded to indicate capacity levels (green for available beds, yellow for nearing capacity, red for full). Another section tracks the flow of patients through the hospital, from emergency room admission to discharge, with visual representations of wait times at each stage. A third section shows predicted patient volumes for the next 24 hours, based on predictive modeling, allowing staff to proactively adjust staffing levels. This dashboard integrates data from various sources – EHRs, scheduling systems, and real-time patient monitoring devices – providing a comprehensive overview of hospital operations and allowing for timely interventions to optimize resource allocation and improve patient flow. This integrated view eliminates information silos, enabling more informed decision-making and a more efficient workflow.
Developing New Healthcare Technologies and Innovations: How Big Data Is Shaping The Future Of Healthcare

Source: amazonaws.com
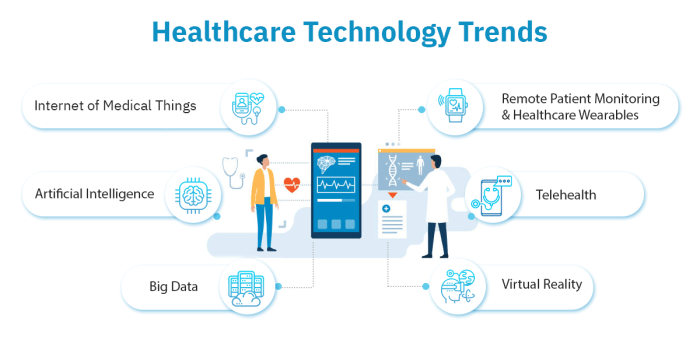
Big data isn’t just reshaping existing healthcare practices; it’s fueling the creation of entirely new technologies and innovations. The sheer volume, velocity, and variety of healthcare data are providing fertile ground for breakthroughs in medical devices, therapies, and diagnostics, ultimately leading to better patient outcomes and a more efficient healthcare system. This section explores how big data is driving this exciting evolution.
The convergence of big data analytics with advancements in other fields like artificial intelligence (AI) and nanotechnology is creating a powerful synergy. This allows researchers and developers to analyze complex datasets, identify patterns previously unseen, and develop innovative solutions to some of healthcare’s most pressing challenges.
Big data’s impact on healthcare is undeniable, revolutionizing diagnostics and treatment. But this wealth of information also presents vulnerabilities, necessitating robust security measures. Understanding how AI combats this is crucial, as seen in the sophisticated techniques detailed in this article on The Role of Artificial Intelligence in Fraud Prevention , which directly translates to safeguarding patient data and ensuring the integrity of the healthcare system.
Ultimately, securing this data is as vital as leveraging it for better care.
Emerging Technologies Driven by Big Data in Healthcare
Big data is the catalyst for a wide range of emerging technologies transforming healthcare. These technologies leverage the power of analytics to improve diagnostics, personalize treatments, and enhance the overall patient experience. For example, wearable sensors continuously collect physiological data, providing real-time insights into a patient’s health. This data, combined with electronic health records (EHRs) and other sources, creates a comprehensive picture that allows for early detection of potential problems and proactive interventions. Another example is the development of sophisticated imaging techniques, like advanced MRI and CT scans, which generate massive datasets that are analyzed using AI algorithms to detect subtle anomalies and improve diagnostic accuracy.
Big Data’s Role in Developing New Medical Devices and Therapies
The development of new medical devices and therapies is significantly accelerated by big data analysis. By analyzing large datasets of patient information, researchers can identify potential drug targets, design more effective clinical trials, and develop personalized treatments. For instance, in drug discovery, big data is used to identify patterns and correlations between genetic information, lifestyle factors, and disease outcomes, leading to the development of more targeted therapies. Similarly, the design and testing of new medical devices, such as implantable sensors or robotic surgical systems, benefit from data-driven simulations and analyses that optimize performance and safety. Companies like Medtronic utilize big data to improve the design and functionality of their implantable devices, based on data collected from millions of patients worldwide.
Artificial Intelligence and Machine Learning in Healthcare
Artificial intelligence (AI) and machine learning (ML) are rapidly transforming healthcare, fueled by the availability of massive datasets. AI algorithms can analyze medical images with remarkable accuracy, detecting subtle signs of disease that might be missed by the human eye. This leads to earlier and more accurate diagnoses, potentially improving treatment outcomes. Moreover, AI-powered systems can personalize treatment plans based on a patient’s unique genetic makeup, medical history, and lifestyle. For example, AI is used in radiology to assist in the detection of cancerous tumors, and in cardiology to predict the risk of heart attacks. Machine learning models are trained on massive datasets of patient records to predict the likelihood of readmission after discharge, allowing healthcare providers to take proactive steps to prevent it.
Big Data Applications in Genomics and Personalized Medicine
Genomics and personalized medicine are revolutionized by the ability to analyze massive genomic datasets. This allows researchers to identify genetic variations associated with specific diseases, paving the way for targeted therapies and preventive measures. For example, analyzing genomic data can help identify individuals at high risk of developing certain cancers, allowing for early screening and intervention. Furthermore, big data enables the development of personalized cancer therapies, tailoring treatments to the unique genetic profile of each tumor. This approach improves treatment efficacy and reduces side effects. Companies like 23andMe are using big data to provide personalized genetic insights to consumers, empowering them to make informed decisions about their health.
Challenges and Opportunities Presented by Big Data in Healthcare Innovation
While big data offers immense potential for healthcare innovation, several challenges must be addressed.
- Data Security and Privacy: Protecting patient data is paramount. Robust security measures are essential to prevent breaches and ensure compliance with regulations like HIPAA.
- Data Interoperability: The lack of standardization in healthcare data formats hinders the seamless sharing and integration of information across different systems.
- Data Bias and Fairness: AI algorithms trained on biased data can perpetuate existing health disparities. Efforts must be made to ensure fairness and equity in the development and application of AI-powered healthcare tools.
- Ethical Considerations: The use of AI in healthcare raises ethical concerns regarding accountability, transparency, and the potential for job displacement.
- Computational Resources: Analyzing massive healthcare datasets requires significant computational power and expertise.
Despite these challenges, the opportunities are substantial. Big data has the potential to accelerate the development of life-saving treatments, improve diagnostic accuracy, and create a more efficient and equitable healthcare system. Addressing these challenges proactively will unlock the full transformative power of big data in healthcare innovation.
Addressing Health Disparities and Improving Access to Care

Source: silstonegroup.com
Big data analytics offers a powerful lens through which we can examine and ultimately dismantle healthcare inequalities. By analyzing vast datasets encompassing demographics, socioeconomic factors, medical histories, and geographic locations, we can identify previously unseen patterns and trends that reveal disparities in access to quality care. This understanding forms the bedrock for developing targeted interventions and strategies aimed at promoting health equity.
Identifying and Addressing Health Disparities
Big data allows for the identification of health disparities based on factors like race, ethnicity, socioeconomic status, geographic location, and insurance coverage. For example, analyzing claims data can reveal significant differences in the types of care received, the frequency of preventative screenings, and overall health outcomes across different demographic groups. This data-driven approach goes beyond anecdotal evidence, providing quantifiable proof of existing disparities and guiding resource allocation towards the most vulnerable populations. The ability to pinpoint specific areas and populations most affected allows for the creation of highly targeted interventions.
Improving Access to Healthcare in Underserved Communities
Improving access to care in underserved communities often involves overcoming significant logistical and socioeconomic barriers. Big data can help identify these barriers. For instance, predictive modeling can forecast areas with high risk of health problems but limited access to healthcare facilities. This information can guide the strategic placement of mobile clinics, telehealth initiatives, or community health centers. Furthermore, analyzing patient travel patterns can inform the development of transportation assistance programs. The aim is to make healthcare services more readily available and accessible to those who need them most.
Examples of Big Data in Public Health Interventions
The use of big data in designing and evaluating public health interventions is rapidly expanding. For example, during a flu outbreak, analysis of social media data can identify the spread of the virus in real-time, allowing for faster and more targeted responses. Similarly, analyzing data from wearable devices and electronic health records can provide insights into the effectiveness of various disease prevention and management programs. These data-driven evaluations allow for the refinement of public health strategies, maximizing their impact and ensuring resource efficiency. A real-world example is the use of big data to track and predict opioid addiction rates in specific regions, leading to better targeted prevention and treatment programs.
Big Data’s Role in Promoting Health Equity
Big data’s potential to promote health equity is immense. By identifying disparities, predicting health risks, and guiding resource allocation, it empowers healthcare providers and policymakers to implement targeted interventions and ultimately reduce health inequalities. This includes developing culturally sensitive healthcare programs, tailoring interventions to specific community needs, and continuously monitoring the effectiveness of these initiatives. The ultimate goal is to create a healthcare system that is equitable and provides everyone with equal opportunities to achieve optimal health outcomes, regardless of their background or circumstances.
Impact of Big Data on Healthcare Access and Quality
| Aspect | Positive Impact | Challenges | Example |
|---|---|---|---|
| Access to Care | Improved identification of underserved communities, optimized resource allocation, increased telehealth utilization | Data privacy concerns, digital literacy disparities, infrastructure limitations | Targeted mobile clinic deployments in rural areas based on predictive modeling of health needs. |
| Quality of Care | Enhanced diagnostics, personalized treatment plans, improved disease surveillance | Data bias, algorithmic fairness issues, lack of interoperability between systems | Early detection of potential heart failure through analysis of electronic health records. |
| Cost Efficiency | Reduced hospital readmissions, optimized resource allocation, improved preventative care | High cost of data storage and analysis, need for skilled data scientists | Predictive modeling to identify patients at high risk of readmission, allowing for proactive intervention. |
| Health Equity | Identification and mitigation of health disparities, targeted interventions for vulnerable populations | Addressing data bias, ensuring equitable access to technology and digital literacy | Development of culturally appropriate health education programs based on community-specific data. |
Final Review
Source: kmgus.com
The integration of big data into healthcare is no longer a futuristic fantasy; it’s a rapidly evolving reality. We’ve explored the transformative power of data analytics in improving diagnostics, personalizing care, optimizing resources, and fostering innovation. While challenges remain, particularly concerning data privacy and ethical considerations, the potential benefits for patients and the healthcare system as a whole are undeniable. The future of healthcare is data-driven, and it’s a future worth embracing.
