How 3D Printing is Shaping the Future of Healthcare? Forget clunky, one-size-fits-all solutions. We’re talking personalized medicine, where 3D printing crafts custom prosthetics, bioprints tissues, and even designs revolutionary drug delivery systems. It’s not just sci-fi anymore; it’s revolutionizing surgeries, streamlining diagnostics, and even transforming how we teach future doctors. Get ready for a deep dive into this incredible tech and its impact on the medical world.
From creating incredibly precise anatomical models for complex surgeries to bioprinting personalized implants and even designing intricate drug delivery systems, 3D printing is rapidly changing the healthcare landscape. This technology isn’t just improving existing processes; it’s opening up entirely new possibilities in personalized medicine, surgical planning, and drug development. The potential is vast, and the implications are profound, promising a future where healthcare is more efficient, precise, and ultimately, more life-saving.
Personalized Medicine and Prosthetics: How 3D Printing Is Shaping The Future Of Healthcare
Source: ourcrowd.com
The healthcare landscape is undergoing a radical transformation, and 3D printing is at the forefront of this revolution. Its ability to create highly customized medical devices and implants is reshaping how we approach treatment, particularly in the realm of personalized medicine and prosthetics. This technology allows for a level of precision and customization previously unimaginable, leading to better patient outcomes and improved quality of life.
3D printing allows for the creation of prosthetics tailored to the exact specifications of each patient. This is a significant advancement over traditional methods, which often involve using generic, off-the-shelf components that may not perfectly fit the individual’s anatomy. This mismatch can lead to discomfort, reduced functionality, and even long-term health problems. The ability to create a truly personalized prosthetic, however, drastically improves comfort, fit, and the overall effectiveness of the device.
Customized Prosthetics
The process begins with a detailed 3D scan of the patient’s limb. This data is then used to design a custom prosthetic that perfectly matches the patient’s unique anatomy. The design can incorporate features such as specialized sockets, articulations, and even customizable cosmetic coverings to match the patient’s skin tone and texture. Different materials, from lightweight plastics to durable metals, can be selected based on the patient’s specific needs and activity levels. This level of personalization ensures a far more comfortable and functional prosthetic, significantly improving the patient’s quality of life. For example, a marathon runner might require a lighter, more flexible prosthetic leg compared to someone with less physically demanding needs. The material choice and design elements can be fine-tuned to suit those individual requirements.
3D Bioprinting and Personalized Implants
Beyond prosthetics, 3D bioprinting is pushing the boundaries of personalized medicine by allowing for the creation of personalized implants and tissues. This technology involves using living cells and biomaterials to construct functional tissues and organs. While still in its early stages, 3D bioprinting holds immense potential for creating customized implants for bone grafts, cartilage repair, and even the creation of personalized organ transplants. Imagine a future where a patient requiring a bone graft receives a perfectly matched, bioprinted graft, minimizing the risk of rejection and promoting faster healing. This represents a huge leap forward in surgical procedures, offering more effective and less invasive treatment options. For instance, research is already underway using 3D bioprinting to create personalized skin grafts for burn victims, dramatically improving their healing process and reducing scarring.
Cost-Effectiveness of 3D-Printed Prosthetics
While the initial investment in 3D printing technology can be substantial, the long-term cost-effectiveness can be significant. The ability to create custom prosthetics on demand reduces reliance on large inventories of pre-fabricated components and significantly reduces waste. Moreover, the improved fit and functionality of 3D-printed prosthetics can lead to reduced healthcare costs associated with revisions, replacements, and complications from poorly fitting prosthetics.
| Prosthetic Type | Cost (USD) | Production Time (Weeks) | Patient-Specific Fit |
|---|---|---|---|
| Traditional Below-Knee Prosthesis | $10,000 – $20,000 | 4-8 | Moderate; adjustments often required |
| 3D-Printed Below-Knee Prosthesis | $8,000 – $15,000 | 2-4 | Excellent; highly customized |
| 3D-Bioprinted Bone Graft (estimated) | $5,000 – $15,000 | Variable, dependent on complexity | Exceptional; genetically matched |
*Note: Cost estimates are approximate and vary depending on materials, complexity, and location.*
Surgical Planning and Tools
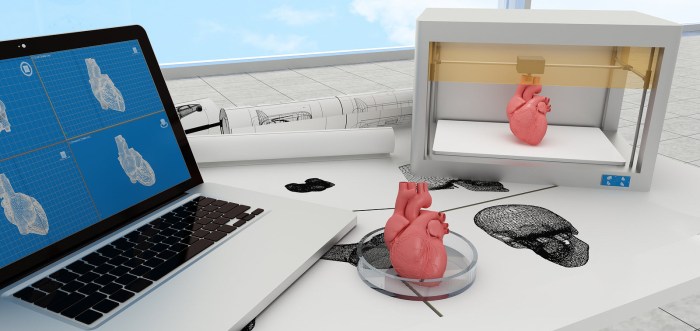
Source: nridigital.com
3D printing is revolutionizing surgical practices, moving beyond creating personalized prosthetics and medications. Its impact on surgical planning and the development of innovative tools is reshaping the operating room, leading to safer, more precise, and less invasive procedures. The ability to create highly accurate anatomical models and customized instruments is transforming the surgical landscape.
The creation of patient-specific anatomical models using 3D printing is a game-changer for surgical planning. Surgeons can now hold a physical representation of a patient’s anatomy, allowing for a more thorough pre-operative assessment. This detailed model allows for better visualization of complex structures, identification of potential challenges, and the planning of precise incisions and implant placement. This pre-operative planning reduces surgical time, minimizes complications, and improves overall patient outcomes. Imagine a neurosurgeon planning a complex brain surgery with a 3D printed model of the patient’s skull and brain – the level of detail and precision achieved is unmatched by traditional methods.
3D-Printed Surgical Instruments and Tools
3D printing allows for the creation of highly customized surgical instruments tailored to the specific needs of a procedure. These instruments can be designed with intricate features and geometries that are impossible to achieve with traditional manufacturing methods. For example, surgeons can create instruments with specialized grips, angles, and sizes to access difficult-to-reach areas during minimally invasive surgery. The advantages over traditional instruments include improved precision, enhanced ergonomics, and reduced invasiveness, leading to faster recovery times and reduced patient trauma. One example is the creation of custom bone cutting guides for orthopedic surgery, ensuring precise bone cuts and implant placement. Another is the development of complex forceps with customized gripping mechanisms for delicate procedures like microsurgery.
Impact on Surgical Training and Education, How 3D Printing is Shaping the Future of Healthcare
The use of 3D-printed models significantly enhances surgical training and education.
The availability of realistic anatomical models allows surgical trainees to practice complex procedures in a risk-free environment. This hands-on experience improves their technical skills and decision-making abilities before operating on real patients. Furthermore, 3D-printed models can be used to simulate various surgical scenarios, including complications, enabling trainees to develop problem-solving skills and improve their preparedness for real-world situations. These models also provide an invaluable tool for teaching anatomy and surgical techniques, offering a more engaging and interactive learning experience compared to traditional methods. The ability to manipulate and study the models offers a deeper understanding of anatomical structures and their relationships, leading to improved surgical skills and patient care.
- Improved surgical technique through hands-on practice on realistic models.
- Enhanced understanding of complex anatomical structures and relationships.
- Development of problem-solving skills through simulation of various surgical scenarios.
- Reduced reliance on cadavers for anatomical training, offering a more sustainable and ethical alternative.
- Cost-effective method for creating reusable training models, reducing the overall training expenses.
Drug Delivery and Pharmaceuticals
3D printing is revolutionizing drug delivery, moving beyond the limitations of traditional methods to create highly personalized and efficient systems. This technology allows for the creation of intricate structures and the precise control of drug release, paving the way for more effective treatments and improved patient outcomes. The ability to tailor drug delivery to individual needs promises a future where medications are not just more effective, but also safer and more convenient.
The use of 3D printing in pharmaceuticals extends beyond simply creating pills. It’s about designing and manufacturing complex delivery systems that precisely control the release of medication over time and target specific areas of the body. This level of control is crucial for treating chronic diseases where consistent, controlled drug levels are necessary, and also for minimizing side effects by delivering drugs only where needed. This personalized approach is transforming how we approach medication administration, leading to better patient compliance and therapeutic efficacy.
Personalized Drug Delivery Systems
3D printing enables the creation of personalized drug delivery systems tailored to individual patient needs and disease characteristics. Imagine a tiny, biodegradable implant, precisely designed and 3D-printed to release a specific medication at a predetermined rate over several weeks or months. This contrasts sharply with traditional methods, such as daily pills or injections, which can lead to inconsistent drug levels and potential side effects. For example, a patient with a slow-release medication implant might experience fewer fluctuations in their blood medication levels, leading to better disease management and reduced risk of adverse events. The ability to customize the shape, size, and material of the implant allows for targeted drug delivery to specific organs or tissues, maximizing therapeutic benefits and minimizing off-target effects. This precision offers a significant advantage over systemic drug delivery, which can lead to side effects in healthy tissues.
3D-Printed Scaffolds for Tissue Engineering and Drug Release
3D-printed scaffolds provide a structural framework for tissue regeneration, acting as a template for cells to grow and rebuild damaged tissues. These scaffolds can be designed with intricate pore structures to optimize cell growth and vascularization. More importantly, these scaffolds can be infused with drugs, creating a controlled-release system that promotes tissue regeneration while simultaneously minimizing inflammation or scarring. For instance, a scaffold designed for bone regeneration could be loaded with bone growth factors and antibiotics, ensuring a supportive environment for healing while combating infection. The precise control over drug release offered by 3D-printed scaffolds significantly enhances the efficacy of tissue engineering therapies, leading to faster healing times and improved functional outcomes.
Hypothetical 3D-Printed Drug Delivery System for Type 1 Diabetes
Consider a 3D-printed insulin delivery system for managing Type 1 diabetes. This system would consist of a small, biocompatible implant, perhaps shaped like a tiny capsule, implanted subcutaneously. The implant would be composed of a biodegradable polymer matrix containing insulin microspheres. The microspheres would be designed to release insulin at a rate controlled by the patient’s glucose levels, monitored via a small, integrated glucose sensor. The sensor would communicate wirelessly with a small external device that would adjust the insulin release rate accordingly. The implant’s structure could be optimized for optimal biocompatibility and minimal immune response. This system would provide a continuous and personalized insulin delivery, eliminating the need for multiple daily injections and greatly improving glycemic control, reducing the long-term complications associated with diabetes. The system’s design would incorporate features to facilitate easy replacement or removal as needed, ensuring patient safety and comfort.
Medical Imaging and Diagnostics
3D printing is revolutionizing medical imaging and diagnostics, moving beyond simple visualization to create tangible, manipulable models that enhance understanding and improve procedures. This technology allows healthcare professionals to better comprehend complex anatomical structures and plan treatments with greater precision, ultimately leading to improved patient outcomes.
The ability to transform digital medical images, such as CT scans and MRIs, into physical 3D models offers a wealth of benefits previously unimaginable. These models provide a level of detail and understanding that traditional 2D images simply can’t match, facilitating better communication and collaboration amongst the healthcare team and, importantly, the patient.
Creating 3D Models from Medical Images
The process begins with acquiring high-resolution medical images (CT scans, MRI, etc.). Specialized software then processes these images, converting the digital data into a 3D model. This digital model is then sent to a 3D printer, which uses various materials (plastics, resins, biocompatible materials) to construct a physical replica of the patient’s anatomy. For example, a surgeon might use a 3D-printed model of a patient’s skull to plan a complex craniotomy, allowing for a more accurate and less invasive procedure. Similarly, a cardiologist might utilize a 3D-printed model of a heart with a congenital defect to better understand the anomaly and plan the optimal surgical approach. The detail achievable allows for precise measurements and the identification of subtle features that might be missed on a screen.
Benefits for Patient Education and Communication
3D-printed models offer unparalleled tools for patient education and improved communication between patients and healthcare providers. Holding a physical model of their own anatomy allows patients to better grasp their condition and treatment plan. This visual aid helps bridge the communication gap often present between medical professionals and patients who may lack a strong medical background. For example, a patient facing a complex surgery can better understand the procedure’s scope and potential risks by examining a 3D model of their affected area. This leads to improved patient compliance and reduced anxiety. Furthermore, the models can be used in consultations with multiple specialists, ensuring everyone is on the same page and working towards a unified treatment strategy.
Improving the Accuracy and Efficiency of Diagnostic Procedures
3D printing significantly improves the accuracy and efficiency of diagnostic procedures. Pre-surgical planning becomes dramatically enhanced; surgeons can rehearse procedures on the 3D model, identify potential challenges, and refine their surgical technique. This reduces operating time, minimizes complications, and ultimately leads to better patient outcomes. Moreover, the models can be used for educational purposes, training medical students and residents in a safe and controlled environment. The creation of customized surgical guides and instruments based on the 3D models further improves the precision and efficiency of procedures. For instance, a 3D-printed guide can ensure the precise placement of implants during orthopedic surgery, reducing the risk of complications and improving the success rate. The ability to create these customized tools significantly reduces operating time and enhances the overall surgical experience.
Challenges and Future Directions
3D printing in healthcare is rapidly evolving, but it’s not without its hurdles. While the potential benefits are immense, several challenges need to be addressed before widespread adoption becomes a reality. Overcoming these obstacles will unlock even greater advancements in personalized medicine and improve patient care significantly.
The current landscape of 3D printing in healthcare faces a number of limitations, hindering its full potential. These challenges are intertwined and require a multi-faceted approach for resolution.
Material Limitations and Regulatory Hurdles
One significant constraint is the limited range of biocompatible and clinically approved materials suitable for 3D printing in medical applications. Many promising materials are still undergoing rigorous testing and regulatory approval processes, which can be lengthy and expensive. For instance, the development of a new bioink for organ bioprinting requires extensive research to ensure biocompatibility, sterility, and efficacy. Furthermore, regulatory bodies like the FDA have strict guidelines for medical devices, demanding rigorous testing and documentation before approval, creating a bottleneck for the adoption of novel 3D-printed medical products. This regulatory landscape adds complexity and cost, slowing down the translation of research into clinical practice. Streamlining the regulatory process and accelerating material development are crucial for overcoming this challenge.
Potential Future Applications of 3D Printing in Healthcare
Despite current limitations, the future of 3D printing in healthcare looks incredibly promising. The technology is poised to revolutionize various aspects of medical practice, pushing the boundaries of what’s possible. One of the most exciting frontiers is organ bioprinting. Scientists are working on creating functional organs using 3D bioprinting techniques, potentially solving the critical shortage of donor organs. This involves precisely layering cells and biomaterials to create complex tissue structures that mimic the architecture and function of human organs. While still in its early stages, this research holds immense potential to transform organ transplantation and significantly improve patient outcomes. Beyond organ bioprinting, personalized therapies are also on the horizon. 3D printing allows for the creation of customized implants, prosthetics, and drug delivery systems tailored to individual patient needs and anatomy. This level of personalization offers the potential for improved treatment efficacy and reduced side effects. For example, customized drug delivery systems can ensure that medication reaches its target site efficiently, minimizing systemic exposure and potential side effects.
Predicted Growth of 3D Printing in Healthcare
Imagine a graph charting the growth of 3D printing in healthcare over the next decade. The line starts relatively flat, reflecting the current state, with a gradual incline representing the steady adoption of existing applications like surgical guides and prosthetics. Then, around the midpoint of the decade, the line sharply accelerates upwards, mirroring the breakthroughs in bioprinting and personalized therapies. This steep rise is fueled by successful clinical trials demonstrating the efficacy and safety of bioprinted tissues and organs, alongside regulatory approvals for new biocompatible materials. By the end of the decade, the line plateaus at a significantly higher level, indicating widespread integration of 3D printing across various healthcare sectors. This projection isn’t just speculation; it’s driven by the ongoing advancements in materials science, bioengineering, and regulatory frameworks. For instance, companies like Organovo and Prellis Biologics are making significant strides in bioprinting, and increasing investments in research and development further solidify this predicted growth. The successful implementation of even a few major bioprinting breakthroughs would dramatically alter the landscape, driving substantial growth within the projected timeframe.
Last Word
The future of healthcare is undeniably intertwined with the advancements in 3D printing technology. We’ve seen how this innovative approach is personalizing treatments, enhancing surgical precision, and accelerating drug development. While challenges remain, the potential for 3D printing to revolutionize healthcare is undeniable. Imagine a future where organ bioprinting becomes a reality, personalized therapies are commonplace, and healthcare is more accessible and effective than ever before. The journey is just beginning, and the possibilities are truly breathtaking.
