How AI is Shaping the Future of Predictive Health Monitoring Systems? Forget crystal balls; the future of healthcare is algorithmic. AI is no longer a futuristic fantasy—it’s actively revolutionizing how we predict, prevent, and manage illnesses. From analyzing wearable sensor data to deciphering complex medical images, artificial intelligence is empowering healthcare professionals with unprecedented insights, paving the way for personalized medicine and proactive healthcare interventions. This isn’t just about predicting who might get sick; it’s about crafting tailored strategies to keep people healthy, longer.
This deep dive explores the diverse applications of AI in predictive health, examining the algorithms driving the change, the ethical considerations involved, and the exciting possibilities that lie ahead. We’ll uncover how AI is transforming various medical fields, improving diagnostic accuracy, and ultimately, enhancing patient outcomes. Get ready to witness the future of healthcare, one algorithm at a time.
AI Algorithms in Predictive Health Monitoring

Source: appstudio.ca
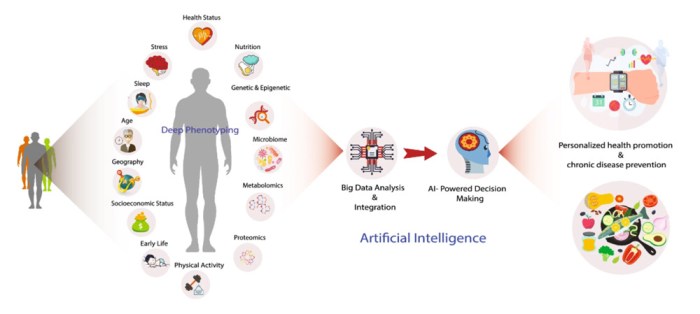
Predictive health monitoring is undergoing a revolution thanks to the power of artificial intelligence. AI algorithms are no longer a futuristic fantasy; they’re actively analyzing vast datasets to identify patterns and predict health risks, paving the way for proactive and personalized healthcare. This allows for earlier interventions, potentially preventing serious illnesses and improving overall health outcomes. Let’s delve into the specific algorithms driving this change.
Machine Learning Algorithms in Predictive Health
Machine learning (ML) forms the backbone of many predictive health systems. These algorithms learn from data without explicit programming, identifying complex relationships that might be missed by human analysis. Various ML techniques are employed, each with its strengths and weaknesses. For instance, support vector machines (SVMs) are effective in classifying patients into risk categories based on their medical history and lifestyle factors. Random forests, on the other hand, can handle high-dimensional data and provide insights into the relative importance of different risk factors in predicting a specific outcome, like the likelihood of a heart attack. Logistic regression is a simpler, yet powerful method used frequently for binary classification tasks, such as predicting the probability of a patient developing diabetes based on their blood glucose levels and other relevant factors.
Deep Learning Algorithms in Predictive Health
Deep learning (DL), a subset of machine learning, utilizes artificial neural networks with multiple layers to analyze complex data. Its ability to automatically learn intricate features from raw data makes it particularly suitable for analyzing medical images (X-rays, CT scans) and wearable sensor data. Convolutional neural networks (CNNs) excel at image recognition, aiding in the early detection of diseases like cancer by identifying subtle anomalies in medical scans. Recurrent neural networks (RNNs), especially Long Short-Term Memory (LSTM) networks, are adept at handling sequential data like electrocardiograms (ECGs) to detect arrhythmias or predict seizure onset in epilepsy patients. These algorithms have demonstrated impressive accuracy in various applications, often surpassing traditional methods.
Comparing and Contrasting Algorithm Performance
The performance of different AI algorithms varies depending on the specific health outcome being predicted and the nature of the data. While deep learning models often achieve higher accuracy on complex tasks like image analysis, they require significantly more data for training and are computationally more expensive than simpler ML algorithms. For example, in predicting the risk of cardiovascular disease, a study might show that a deep learning model trained on a large dataset of electronic health records achieves a higher area under the ROC curve (AUC) compared to a logistic regression model trained on the same data. However, the logistic regression model might be more interpretable, offering insights into the relative importance of individual risk factors. The choice of algorithm involves a trade-off between accuracy, interpretability, computational cost, and data availability.
The Role of Big Data and Data Analytics
The accuracy and effectiveness of AI algorithms in predictive health are inextricably linked to the quality and quantity of data used for training. Big data, encompassing diverse data types, fuels the development of these powerful predictive models.
Genomic Data
Genomic data, including an individual’s DNA sequence, provides valuable insights into genetic predispositions to certain diseases. Integrating genomic data with other health information allows for more personalized risk assessments and tailored preventive measures. For instance, identifying specific genetic markers associated with an increased risk of breast cancer can lead to earlier screening and more targeted interventions.
Wearable Sensor Data
Wearable devices like smartwatches and fitness trackers generate continuous streams of physiological data, including heart rate, activity levels, and sleep patterns. This data, when combined with other information, can provide a comprehensive picture of an individual’s health status and identify subtle changes that might indicate an impending health issue. For example, changes in heart rate variability detected by a smartwatch could be an early warning sign of a developing cardiovascular problem.
Electronic Health Records (EHRs), How AI is Shaping the Future of Predictive Health Monitoring Systems
EHRs contain a wealth of information on patients’ medical history, including diagnoses, medications, and lab results. Analyzing EHR data can reveal patterns and risk factors associated with various diseases. For instance, identifying patients with a combination of risk factors for heart failure allows for proactive interventions to prevent hospitalizations. However, EHR data can be incomplete, inconsistent, and subject to biases, requiring careful cleaning and preprocessing before use in AI algorithms. The integration of these different data types is crucial for building comprehensive and accurate predictive models.
Data Sources and Integration in Predictive Health

Source: aicontroversy.com
Predictive health monitoring systems rely on a rich tapestry of data to weave their insightful predictions. The accuracy and effectiveness of these systems are directly tied to the quality, diversity, and seamless integration of this data. Understanding the sources, potential biases, and challenges involved in combining this information is crucial for developing truly impactful predictive health solutions.
The power of predictive health lies in its ability to analyze diverse data streams to identify patterns and risks. However, integrating these diverse sources presents significant hurdles. This section delves into the key data sources, the challenges of integration, and strategies for building robust and reliable predictive health systems.
Data Sources and Potential Biases
Predictive health monitoring systems draw upon a variety of data sources, each offering unique insights but also presenting unique challenges. Below is a comparison of key data types, sources, and potential biases:
| Data Type | Source | Potential Biases | Example |
|---|---|---|---|
| Wearable Sensor Data (Heart rate, activity levels, sleep patterns) | Smartwatches, Fitness Trackers | Sampling bias (users may be healthier/more tech-savvy), device accuracy, data incompleteness (missed recordings) | A fitness tracker might inaccurately record heart rate during intense exercise, leading to biased data. |
| Electronic Health Records (EHRs) | Hospitals, Clinics | Data entry errors, missing data, inconsistencies in coding, selection bias (patients seeking care may differ from the general population) | Inconsistent recording of blood pressure readings across different clinics can skew population-level analysis. |
| Medical Imaging Data (X-rays, CT scans, MRIs) | Imaging Centers, Hospitals | Image quality variations, inter-reader variability (differences in interpretation by radiologists), access disparities (unequal access to imaging technologies) | Differences in image resolution across different imaging facilities can affect the accuracy of AI-driven diagnoses. |
| Genomic Data | Genetic testing labs | Population stratification (differences in genetic makeup across populations), interpretation bias (variation in how genetic information is understood and applied), privacy concerns | Genetic risk scores might overestimate risk in certain populations due to limited representation in the training data. |
Challenges and Solutions in Data Integration and Interoperability
Integrating data from disparate sources presents several significant challenges. Data standardization, security, and privacy are paramount concerns.
One major challenge is the lack of interoperability between different systems. Different healthcare providers and devices often use different data formats and standards, making it difficult to combine and analyze data effectively. Solutions include the adoption of standardized data formats (like FHIR) and the development of robust data integration platforms that can handle diverse data types. Ensuring data quality is also critical; this involves implementing data validation and cleaning procedures to identify and correct errors.
Data security and privacy are paramount. Robust security measures, including encryption and access control, are essential to protect sensitive patient information. Compliance with regulations like HIPAA is crucial.
Hypothetical Data Integration Architecture
A robust data integration architecture for a predictive health monitoring system would involve several key components:
Data from wearables, EHRs, and medical imaging systems would be ingested into a secure data lake. This data lake would act as a central repository for all raw data. A data integration engine would then transform and standardize the data, ensuring consistency and compatibility. This involves cleaning, transforming, and validating data using various techniques like data mapping and ETL (Extract, Transform, Load) processes. The cleaned and standardized data would then be loaded into a data warehouse, optimized for analytical queries. Finally, AI algorithms would access the data in the data warehouse to generate predictions and insights. The entire system would be designed with robust security and privacy measures, adhering to relevant regulations and best practices.
Applications of AI in Specific Health Areas
Source: wipro.com
AI’s predictive power is revolutionizing healthcare, moving beyond reactive treatment to proactive prevention and personalized care. By analyzing vast datasets and identifying subtle patterns, AI algorithms are transforming how we approach various health challenges, leading to earlier diagnoses, more effective treatments, and ultimately, better patient outcomes. This section will delve into specific applications across different medical specialties, showcasing AI’s transformative impact.
AI in Cardiology: Predicting Heart Failure
AI is proving invaluable in cardiology, particularly in predicting heart failure, a leading cause of death globally. Machine learning algorithms, trained on extensive datasets encompassing patient medical history, electrocardiograms (ECGs), echocardiograms, and blood test results, can identify individuals at high risk of developing heart failure. For example, a convolutional neural network (CNN) might analyze ECG patterns to detect subtle irregularities indicative of impending heart failure, while a recurrent neural network (RNN) could analyze temporal trends in patient data to predict the likelihood of an event within a specific timeframe. The use of such AI-driven predictive models allows for early intervention, lifestyle modifications, and timely medication adjustments, ultimately improving patient survival rates and reducing hospital readmissions. One study demonstrated that an AI model achieved an accuracy rate of over 85% in predicting heart failure within a year, significantly outperforming traditional risk assessment methods.
AI in Oncology: Cancer Risk Prediction and Treatment Response
The application of AI in oncology holds immense promise, particularly in improving cancer risk prediction and personalizing treatment strategies. AI algorithms can analyze genomic data, medical imaging (like CT scans and MRIs), and patient lifestyle factors to assess an individual’s risk of developing specific cancers. For instance, an AI model might analyze a patient’s genetic profile to identify mutations associated with increased breast cancer risk, allowing for proactive screening and early detection. Furthermore, AI can predict a tumor’s response to different therapies, guiding oncologists in selecting the most effective treatment plan for each patient. A hypothetical case study: Imagine a patient diagnosed with lung cancer. An AI model, analyzing the patient’s tumor biopsy and genetic data, predicts a high likelihood of response to immunotherapy. This information allows the oncologist to tailor the treatment plan, potentially avoiding ineffective and toxic chemotherapy regimens, thereby improving the patient’s quality of life and chances of survival. Real-world examples demonstrate that AI-powered tools are already improving cancer diagnosis accuracy and treatment personalization, leading to better patient outcomes.
AI in Diabetes Management: Predicting Complications and Personalizing Treatment
AI is transforming diabetes management by enabling more precise prediction of complications and facilitating personalized treatment plans. By analyzing continuous glucose monitoring (CGM) data, wearable sensor data, lifestyle information, and medical history, AI algorithms can predict the likelihood of developing diabetic retinopathy, nephropathy, or neuropathy. For example, an AI model might identify patterns in CGM data that indicate a high risk of hypoglycemic episodes, allowing for timely adjustments to insulin dosages and preventative measures. Moreover, AI can personalize treatment plans based on individual patient characteristics and preferences. Consider a hypothetical scenario: A patient with type 1 diabetes uses a smart insulin pen integrated with an AI-powered system. The system analyzes the patient’s CGM data, activity levels, and dietary habits to automatically adjust insulin delivery, minimizing blood glucose fluctuations and reducing the risk of complications. This personalized approach, enabled by AI, enhances diabetes management and improves patient quality of life.
Ethical and Societal Implications
The integration of AI into predictive health monitoring systems, while promising revolutionary advancements, necessitates a careful consideration of its ethical and societal ramifications. The potential benefits are immense, but realizing them responsibly requires a proactive approach to addressing potential pitfalls. Ignoring these implications could lead to unintended consequences, undermining public trust and hindering the equitable distribution of these powerful technologies.
The use of AI in healthcare introduces a complex web of ethical considerations and potential societal impacts. Balancing innovation with responsible implementation is crucial to ensuring that these technologies benefit everyone fairly and ethically.
Data Privacy and Security Concerns
The vast amounts of sensitive personal health data required to train and operate AI predictive health systems raise significant privacy concerns. Data breaches could expose individuals to identity theft, discrimination, or even physical harm. Robust data anonymization techniques, secure storage protocols, and transparent data governance frameworks are essential to mitigating these risks. For example, the implementation of differential privacy techniques can help mask individual data points while still allowing for meaningful aggregate analysis. Furthermore, strong encryption and access control mechanisms are critical to preventing unauthorized access to sensitive patient information.
Algorithmic Bias and Fairness
AI algorithms are trained on data, and if that data reflects existing societal biases, the resulting algorithms will likely perpetuate and even amplify those biases. This can lead to unfair or discriminatory outcomes, particularly for marginalized populations. For instance, an algorithm trained primarily on data from one demographic group might perform poorly or inaccurately when applied to another, leading to misdiagnosis or inappropriate treatment recommendations. Rigorous testing, validation, and ongoing monitoring of algorithms for bias are crucial to ensuring fairness and equity in the application of AI in healthcare.
Informed Consent and Transparency
Patients need to be fully informed about how their data will be used and the potential risks and benefits of AI-powered predictive health systems before consenting to their use. Transparency is key here. Clear and understandable explanations of how algorithms work and the limitations of their predictions are necessary for patients to make truly informed decisions about their participation. This includes explaining the potential for errors and biases in the system, and ensuring that individuals retain control over their data and can withdraw consent at any time.
Societal Impacts of Widespread Adoption
The widespread adoption of AI-powered predictive health systems could significantly impact access to care, healthcare costs, and public health outcomes. While AI has the potential to improve efficiency and accuracy in diagnosis and treatment, it also raises concerns about equitable access to these technologies. Cost considerations, both for development and implementation, could exacerbate existing health disparities, making these advanced tools available only to those with the means to access them. Furthermore, the potential for job displacement among healthcare professionals needs to be addressed proactively through retraining and upskilling initiatives.
AI’s predictive power is revolutionizing healthcare, enabling early disease detection and personalized treatment plans. This same predictive capability extends beyond individual health; consider how AI is optimizing resource allocation and improving urban living, as detailed in this insightful article on The Role of AI in Optimizing Urban Infrastructure and City Planning. Ultimately, these advancements in AI-driven prediction will lead to healthier individuals and more efficient, livable cities.
Framework for Responsible AI Development and Deployment
A robust framework for responsible AI development and deployment in predictive health is essential to mitigate ethical and societal risks. This framework should prioritize transparency, accountability, and fairness. Transparency requires clear documentation of algorithms, data sources, and decision-making processes. Accountability mechanisms are needed to address errors or biases, ensuring that those responsible are held accountable for any negative consequences. Fairness requires ongoing monitoring and evaluation of algorithms to identify and address potential biases, ensuring equitable access to the benefits of AI in healthcare for all populations.
Future Trends and Challenges
Predictive health monitoring, powered by AI, is poised for explosive growth. However, realizing its full potential requires navigating a complex landscape of technological advancements and societal considerations. The next decade will witness a dramatic reshaping of this field, driven by both innovative solutions and the need to address significant hurdles.
The future of AI in predictive health hinges on several key advancements and their seamless integration. We’re not just talking about incremental improvements; we’re looking at a paradigm shift in how we approach healthcare, moving from reactive to proactive care.
Advanced Machine Learning Techniques
The application of more sophisticated machine learning algorithms, such as deep learning and reinforcement learning, will significantly enhance the accuracy and efficiency of predictive models. Deep learning, with its ability to analyze complex, high-dimensional data, will allow for the identification of subtle patterns indicative of disease onset, even before the appearance of overt symptoms. Reinforcement learning will optimize treatment strategies based on individual patient responses, leading to personalized and adaptive healthcare. For example, imagine an AI system that can predict the likelihood of a diabetic patient experiencing a hypoglycemic episode based on their real-time data and then automatically adjust their insulin delivery accordingly.
Integration with IoT and Blockchain
The Internet of Things (IoT) will play a crucial role in gathering the vast amounts of data needed to fuel these advanced algorithms. Wearable sensors, smart implants, and connected medical devices will continuously monitor vital signs, activity levels, and other physiological parameters, providing a rich stream of real-time information. Blockchain technology can enhance data security and privacy, ensuring patient confidentiality while facilitating secure data sharing between healthcare providers. Imagine a system where a patient’s medical data is securely stored on a blockchain, accessible only to authorized personnel, while simultaneously contributing to large-scale research initiatives aimed at improving predictive models.
Regulatory Hurdles and Standardization
The widespread adoption of AI in predictive health faces significant regulatory challenges. Establishing clear guidelines for data privacy, algorithm validation, and liability is crucial to build public trust and ensure responsible innovation. The lack of standardization in data formats and AI algorithms presents another major hurdle. Interoperability between different systems and devices is essential for seamless data integration and efficient healthcare delivery. For instance, different hospitals using different AI systems for cardiac risk prediction would severely hamper the ability to effectively compare and analyze data on a larger scale.
Public Trust and Ethical Considerations
Building public trust is paramount for the successful implementation of AI in predictive health. Addressing concerns about data privacy, algorithmic bias, and the potential for misuse of sensitive information is essential. Transparency in the development and deployment of AI algorithms, along with clear explanations of their decision-making processes, can help to alleviate these concerns. Furthermore, robust ethical frameworks are needed to guide the development and use of AI in healthcare, ensuring that these technologies are used responsibly and equitably. For example, algorithms must be rigorously tested to ensure they do not perpetuate existing health disparities based on factors like race or socioeconomic status.
Anticipated Evolution of AI in Predictive Health (5-10 Years)
Imagine a visual representation: a timeline stretching across five to ten years. At the beginning, we see disparate, siloed systems – individual hospitals and clinics using isolated AI tools. Over time, these systems become increasingly interconnected, facilitated by IoT and blockchain technology. Advanced machine learning techniques, particularly deep learning and reinforcement learning, drive the development of increasingly sophisticated predictive models. The visual representation culminates in a highly integrated, personalized healthcare ecosystem, where AI plays a central role in preventing diseases, personalizing treatments, and improving overall health outcomes. The key technological advancements – advanced machine learning, IoT integration, blockchain security, and improved regulatory frameworks – are depicted as converging forces propelling this evolution. The impact on healthcare is shown through improved patient outcomes, reduced healthcare costs, and a more proactive and personalized approach to care.
Last Point: How AI Is Shaping The Future Of Predictive Health Monitoring Systems
The integration of AI into predictive health monitoring systems marks a pivotal moment in healthcare. While challenges remain, the potential benefits—from earlier disease detection to personalized treatment plans—are undeniable. The future is less about reacting to illness and more about proactively safeguarding health, thanks to the power of AI. As the technology evolves and ethical considerations are addressed, we can anticipate an era of healthcare that’s not only more effective but also more equitable and personalized than ever before. The journey has just begun, and the destination is a healthier future for all.
