The Role of Machine Learning in Personalized Healthcare Treatments is revolutionizing how we approach medicine. Forget the one-size-fits-all approach; we’re diving into a future where treatments are tailored to your unique genetic makeup, lifestyle, and medical history. Machine learning algorithms are crunching massive datasets to diagnose diseases earlier, predict patient outcomes, and even accelerate drug discovery. It’s a game-changer, but it’s not without its challenges – ethical considerations and data privacy are paramount. Let’s explore this fascinating intersection of technology and healthcare.
This journey into personalized medicine reveals how AI is transforming diagnostics, treatment plans, and even the way new drugs are developed. We’ll delve into real-world examples, discuss the ethical implications, and peek into a future where AI empowers healthcare professionals to deliver more precise and effective care. Get ready to be amazed (and maybe a little bit awestruck).
Introduction to Personalized Healthcare and Machine Learning: The Role Of Machine Learning In Personalized Healthcare Treatments
Personalized healthcare, also known as precision medicine, is shifting the focus from treating diseases based on population averages to tailoring treatments to individual patients. This approach considers a patient’s unique genetic makeup, lifestyle, environment, and medical history to optimize treatment strategies. It’s a move away from the “one-size-fits-all” approach that has characterized much of traditional medicine. The current landscape is rapidly evolving, driven by advancements in genomics, data analytics, and, crucially, machine learning.
The integration of machine learning (ML) into healthcare offers a powerful set of tools to analyze complex patient data and improve the effectiveness of personalized treatments. ML algorithms can identify patterns and insights from massive datasets that would be impossible for humans to detect manually. This allows for more accurate diagnoses, prediction of disease risk, and development of tailored therapies. The potential benefits are substantial, leading to improved patient outcomes, reduced healthcare costs, and a more efficient healthcare system.
Benefits of Machine Learning in Personalized Healthcare, The Role of Machine Learning in Personalized Healthcare Treatments
Machine learning algorithms can analyze diverse data sources, including genomic information, electronic health records (EHRs), lifestyle data (e.g., diet, exercise), and imaging data, to create highly individualized patient profiles. This comprehensive view allows for a more precise understanding of a patient’s unique risk factors and potential responses to different treatments. For example, ML models can predict the likelihood of a patient developing a specific disease based on their genetic predispositions and lifestyle factors, enabling early intervention and preventative measures. In cancer treatment, ML is used to analyze tumor characteristics and predict the effectiveness of various chemotherapy regimens, helping oncologists choose the most suitable treatment option for each patient. Similarly, in cardiology, ML algorithms can analyze ECG data to detect subtle patterns indicative of heart disease, leading to earlier diagnosis and improved treatment outcomes.
Challenges and Limitations of Machine Learning in Personalized Healthcare
Despite the immense potential, several challenges hinder the widespread adoption of ML in personalized healthcare. One major obstacle is data availability and quality. ML algorithms require large, high-quality datasets to train effectively. However, access to comprehensive and consistently formatted patient data is often limited due to privacy concerns, data silos, and inconsistencies in data collection methods across different healthcare systems. Furthermore, ensuring data privacy and security is paramount, given the sensitive nature of patient information. Robust data anonymization and security protocols are essential to maintain patient confidentiality and comply with relevant regulations like HIPAA.
Another challenge lies in the interpretability of ML models. Many advanced ML algorithms, such as deep learning models, are often considered “black boxes,” making it difficult to understand how they arrive at their predictions. This lack of transparency can raise concerns about trust and acceptance among clinicians, who need to understand the rationale behind treatment recommendations. The development of more explainable AI (XAI) methods is crucial to address this issue and build confidence in the use of ML in clinical decision-making. Finally, the integration of ML tools into existing healthcare workflows requires significant effort and investment in infrastructure, training, and change management. Successfully implementing ML-based solutions requires collaboration between data scientists, clinicians, and healthcare administrators.
Applications of Machine Learning in Diagnostics
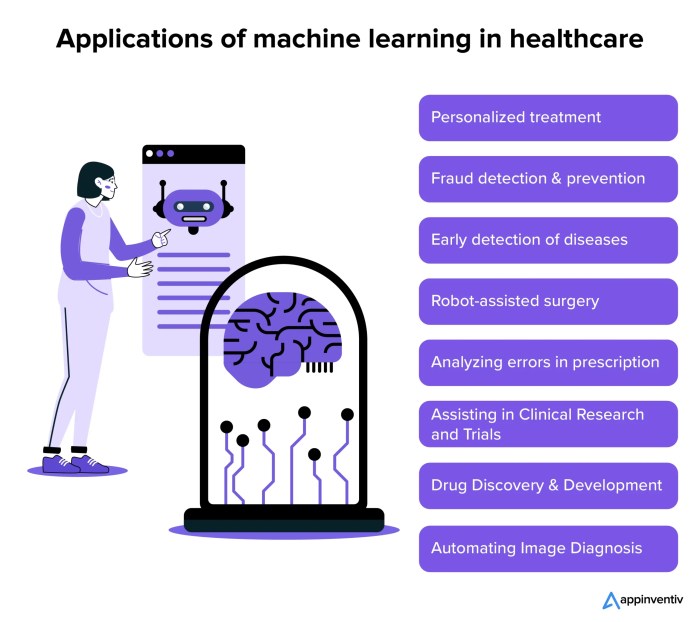
Source: appinventiv.com
Machine learning is revolutionizing healthcare, tailoring treatments to individual genetic profiles and lifestyles. This level of personalization hinges on secure data management, which is why understanding how technology is changing the landscape of digital identity, as explored in this insightful article How Technology is Changing the Landscape of Digital Identity , is crucial. Ultimately, robust digital identity systems are essential for the responsible and effective implementation of AI-driven personalized medicine.
Machine learning is revolutionizing medical diagnostics, offering faster, more accurate, and potentially more cost-effective ways to identify diseases. By analyzing complex medical data, these algorithms can detect patterns invisible to the human eye, leading to earlier and more precise diagnoses. This ultimately improves patient outcomes and streamlines healthcare processes.
Traditional diagnostic methods often rely on subjective interpretations of images or tests, potentially leading to inconsistencies and delays. Machine learning algorithms, however, can process vast amounts of data objectively, minimizing human error and improving diagnostic consistency. This enhanced speed and accuracy is particularly crucial in time-sensitive situations, such as diagnosing strokes or certain cancers.
Machine Learning Algorithms for Disease Diagnosis
Several machine learning algorithms are proving highly effective in medical diagnosis. These algorithms leverage different approaches to analyze data and identify patterns indicative of specific diseases. The choice of algorithm depends on the type of data (images, genomic data, patient history, etc.) and the specific diagnostic task.
- Convolutional Neural Networks (CNNs): CNNs excel at analyzing image data, making them ideal for tasks like analyzing medical images (X-rays, CT scans, MRIs) to detect tumors, fractures, or other abnormalities. For instance, a CNN trained on a large dataset of chest X-rays can accurately identify pneumonia with a high degree of accuracy, often surpassing human radiologists in certain scenarios. The network learns to identify subtle visual patterns indicative of the disease, patterns that may be missed by the human eye due to fatigue or limited experience.
- Support Vector Machines (SVMs): SVMs are powerful algorithms capable of classifying data based on complex relationships. They are used in various diagnostic applications, including identifying different types of leukemia based on gene expression data or predicting the likelihood of heart failure based on patient history and clinical measurements. The algorithm creates a hyperplane that optimally separates different disease classes, enabling accurate classification of new patients.
- Random Forests: Random Forests are ensemble learning methods that combine multiple decision trees to improve prediction accuracy. Their robustness and ability to handle high-dimensional data make them suitable for various diagnostic tasks, such as predicting the risk of developing diabetes based on a patient’s lifestyle, genetic factors, and medical history. The algorithm averages the predictions of multiple trees, reducing the impact of individual tree errors and improving overall accuracy.
Comparison of Machine Learning and Traditional Methods
While traditional diagnostic methods remain valuable, machine learning offers several advantages in terms of accuracy and efficiency. Traditional methods often rely on expert interpretation, which can be subjective and prone to errors due to fatigue or individual biases. Machine learning algorithms, on the other hand, provide objective and consistent analysis, reducing inter-observer variability. Furthermore, machine learning can process vast amounts of data much faster than a human, leading to quicker diagnoses and improved workflow efficiency. The accuracy of machine learning algorithms can often exceed that of traditional methods, particularly in complex diagnostic tasks where subtle patterns need to be identified. However, it is crucial to note that machine learning algorithms are tools, and their performance is heavily reliant on the quality and quantity of training data. Poorly trained models can lead to inaccurate or unreliable diagnoses.
Hypothetical Scenario Illustrating Improved Diagnostic Accuracy
Imagine a scenario involving the diagnosis of diabetic retinopathy, a leading cause of blindness in people with diabetes. Traditional diagnosis relies on ophthalmologists manually examining retinal images for signs of the disease, a process that can be time-consuming and prone to errors due to the subtle nature of the early-stage lesions. A machine learning model, specifically a CNN trained on a large dataset of retinal images, could analyze these images much faster and with greater accuracy. In this hypothetical scenario, the machine learning model achieves a 95% accuracy rate in detecting early-stage diabetic retinopathy, compared to an 85% accuracy rate for experienced ophthalmologists. This improvement in accuracy could lead to earlier intervention, preventing vision loss in many patients. The machine learning system doesn’t replace the ophthalmologist but acts as a powerful tool assisting in diagnosis, enabling faster screening and earlier detection of the disease.
Machine Learning for Treatment Personalization
Machine learning (ML) is revolutionizing healthcare by moving beyond one-size-fits-all approaches to treatment. By analyzing vast amounts of patient data, ML algorithms can identify patterns and predict individual responses to different therapies, paving the way for truly personalized medicine. This allows for the tailoring of treatment plans based on a patient’s unique genetic makeup, lifestyle, medical history, and even their environment, leading to more effective and safer outcomes.
ML algorithms can analyze complex datasets encompassing genomic information, medical imaging, electronic health records, and wearable sensor data to create predictive models. These models can then forecast the likelihood of treatment success, identify potential adverse effects, and even optimize dosage regimens for individual patients. This level of precision minimizes trial-and-error, reduces the risk of adverse reactions, and ultimately improves patient outcomes.
Case Studies of Personalized Treatment Using Machine Learning
Several successful applications of machine learning in personalized treatment demonstrate its transformative potential. For instance, in oncology, ML algorithms are used to predict the likelihood of cancer recurrence based on a patient’s tumor characteristics and genetic profile. This information helps oncologists tailor chemotherapy regimens, radiation therapy, or targeted therapies to maximize efficacy and minimize side effects. In another example, ML is being used to predict which patients with heart failure are most likely to benefit from specific interventions, like implantable cardioverter-defibrillators (ICDs), leading to more effective resource allocation and improved patient survival. Furthermore, in the realm of diabetes management, ML algorithms analyze patient data (blood glucose levels, activity levels, diet) to personalize insulin dosing, resulting in better glycemic control and reduced risk of complications.
Ethical Considerations in Using Patient Data for Algorithm Training
The power of ML in personalized healthcare is undeniable, but its reliance on vast quantities of patient data raises significant ethical concerns. Privacy and data security are paramount. Robust anonymization techniques and secure data storage are crucial to protect sensitive patient information from unauthorized access or misuse. Furthermore, the potential for algorithmic bias needs careful consideration. If the training data reflects existing health disparities, the resulting algorithms may perpetuate or even exacerbate these inequalities. For example, an algorithm trained primarily on data from one demographic group might not accurately predict outcomes for patients from other groups. Therefore, rigorous validation and ongoing monitoring of ML algorithms are essential to ensure fairness and equity in their application. Transparency in algorithm development and deployment is also crucial to build trust and accountability. Clear guidelines and regulations are needed to govern the ethical use of patient data in ML-driven healthcare applications, ensuring that the benefits of personalized medicine are accessible and equitable for all.
Drug Discovery and Development with Machine Learning
Source: aqbsolutions.com
The pharmaceutical industry is notoriously slow and expensive. Developing a new drug can take over a decade and cost billions of dollars. Machine learning (ML) offers a powerful toolkit to significantly accelerate and streamline this process, potentially leading to faster access to life-saving medications. By analyzing vast datasets and identifying patterns invisible to the human eye, ML algorithms can predict drug efficacy, toxicity, and other crucial properties, drastically reducing the time and resources required.
Machine learning is revolutionizing drug discovery and development by automating tasks, improving prediction accuracy, and enabling the exploration of a much larger chemical space than ever before possible. This results in faster identification of promising drug candidates, more efficient clinical trials, and ultimately, more effective treatments reaching patients sooner.
Accelerating Drug Discovery Through Machine Learning
ML algorithms are being integrated into every stage of the drug development pipeline, from target identification to clinical trials. In target identification, ML can analyze genomic data to pinpoint disease-related proteins, which then become targets for drug development. During lead optimization, ML models predict the properties of potential drug molecules, allowing researchers to focus on the most promising candidates. Furthermore, ML can analyze patient data to predict treatment response and identify potential adverse effects, thereby improving the design and efficiency of clinical trials. This integrated approach leads to substantial time and cost savings compared to traditional methods.
Comparison of Traditional and Machine Learning-Assisted Drug Development Timelines
The following table illustrates the potential impact of ML on drug development timelines. Note that these are general estimates and actual timelines can vary depending on the specific drug and disease.
| Stage | Traditional Timeline | Machine Learning Timeline | Impact |
|---|---|---|---|
| Target Identification | 3-5 years | 1-2 years | Significant reduction in time and cost due to automated analysis of large datasets. |
| Lead Optimization | 2-4 years | 1-2 years | Faster identification of promising drug candidates through predictive modeling. |
| Preclinical Testing | 2-3 years | 1-2 years | Improved prediction of drug efficacy and toxicity, reducing the number of failed candidates. |
| Clinical Trials | 6-10 years | 4-6 years | Better patient stratification and prediction of treatment response leading to more efficient trials. |
Machine Learning Models in Drug Design and Testing
Various ML models are employed in different stages of drug discovery. For example, support vector machines (SVMs) are used for classification tasks, such as predicting the binding affinity of a drug molecule to its target. Random forests are effective for predicting various drug properties, including toxicity and efficacy. Deep learning models, such as convolutional neural networks (CNNs) and recurrent neural networks (RNNs), are increasingly used for analyzing complex datasets, like images of protein structures or genomic sequences, enabling more sophisticated predictions. Furthermore, Generative Adversarial Networks (GANs) are employed to design novel drug molecules with desired properties, accelerating the process of lead optimization. The choice of model depends on the specific task and the nature of the available data. For instance, analyzing large image datasets of protein structures often benefits from the power of CNNs, while predicting time-series data, like drug concentration over time, might utilize RNNs. The use of these sophisticated models allows for a more comprehensive understanding of the drug development process and the identification of promising drug candidates.
Predictive Modeling for Patient Outcomes
Predictive modeling, powered by machine learning, is revolutionizing healthcare by offering a glimpse into the future of patient health. By analyzing vast amounts of patient data – from medical history and genetic information to lifestyle choices and environmental factors – these models can forecast the likelihood of specific health outcomes, empowering proactive interventions and improved care. This isn’t about replacing doctors; it’s about giving them powerful tools to make more informed decisions.
Machine learning models can predict patient outcomes with remarkable accuracy by identifying patterns and relationships within complex datasets that might be missed by the human eye. These models leverage algorithms like logistic regression, support vector machines, and neural networks to analyze various risk factors and generate probabilities for specific events, such as readmission rates, disease progression, or response to treatment. For example, a model might predict the likelihood of a patient developing heart failure within the next five years based on factors like age, blood pressure, cholesterol levels, and family history. This allows for earlier interventions, like lifestyle modifications or preventative medication, potentially delaying or preventing the onset of the disease.
Improved Resource Allocation and Healthcare Planning Through Predictive Modeling
Predictive modeling significantly enhances resource allocation and healthcare planning. By forecasting patient needs, healthcare systems can optimize staffing levels, allocate beds more efficiently, and manage resources more effectively. For instance, a model predicting a surge in flu cases during a specific period allows hospitals to proactively increase staffing, procure necessary medications, and prepare for an influx of patients. This proactive approach minimizes disruptions, improves patient care, and reduces overall healthcare costs. Similarly, predicting which patients are most at risk of readmission allows hospitals to focus post-discharge interventions on those most likely to need them, reducing unnecessary readmissions and associated costs. This data-driven approach allows for better utilization of resources and improved patient outcomes.
Factors Contributing to the Accuracy of Predictive Models in Healthcare
The accuracy of predictive models hinges on several crucial factors. A model’s effectiveness is directly tied to the quality and completeness of the data it’s trained on.
The following factors significantly influence the accuracy of predictive models:
- Data Quality and Completeness: Accurate, comprehensive, and unbiased data is paramount. Missing data, inconsistencies, or errors can severely impact model performance. The more complete and accurate the data, the better the model’s predictive capabilities.
- Feature Selection: Identifying the most relevant features (variables) to include in the model is critical. Irrelevant or redundant features can introduce noise and reduce accuracy. Careful feature engineering and selection techniques are essential.
- Model Selection and Tuning: Choosing the appropriate machine learning algorithm and carefully tuning its parameters is crucial. Different algorithms perform better with different types of data and problems. Rigorous model evaluation and selection processes are necessary.
- Data Bias Mitigation: Addressing biases present in the data is crucial to ensure fairness and prevent inaccurate predictions for specific patient subgroups. Techniques for bias detection and mitigation are essential for building equitable and reliable models.
- Model Validation and Generalizability: Robust validation techniques, such as cross-validation, are needed to assess the model’s performance on unseen data and ensure its generalizability to real-world scenarios. A model that performs well only on the training data is unlikely to be reliable in practice.
Data Privacy and Security in Personalized Healthcare
The rise of personalized healthcare, fueled by machine learning’s ability to analyze vast datasets, presents a compelling paradox: While it promises revolutionary improvements in patient care, it also raises significant concerns about data privacy and security. The sensitive nature of health information necessitates robust safeguards to protect patient confidentiality and ensure the ethical and responsible use of this powerful technology. Failing to prioritize these aspects risks eroding public trust and hindering the widespread adoption of life-saving innovations.
The ethical and practical implications of using patient data in machine learning algorithms are profound. Every piece of information, from genetic predispositions to lifestyle choices, holds the potential to reveal deeply personal details about an individual. This data must be handled with the utmost care, adhering to stringent security protocols and legal frameworks designed to prevent unauthorized access, misuse, or disclosure. The potential consequences of a data breach – from identity theft to reputational damage and even compromised healthcare – are severe and far-reaching.
Data Confidentiality and Integrity Measures
Maintaining patient data confidentiality and integrity requires a multi-layered approach. This includes implementing robust encryption techniques to protect data both in transit and at rest. Access control mechanisms, such as role-based access control (RBAC), should be implemented to limit access to sensitive information only to authorized personnel. Regular security audits and penetration testing can identify vulnerabilities and ensure the effectiveness of security measures. Furthermore, data anonymization and de-identification techniques can help minimize the risk of re-identification, though perfect anonymization remains a challenge. Finally, rigorous data governance policies and procedures are essential to ensure that data is handled responsibly throughout its lifecycle. For example, a hospital might use differential privacy techniques to add noise to aggregate statistics released for research purposes, making it harder to identify individual patients while still allowing for useful analysis.
Legal and Regulatory Frameworks
The use of patient data in machine learning applications is governed by a complex web of legal and regulatory frameworks. The Health Insurance Portability and Accountability Act (HIPAA) in the United States, the General Data Protection Regulation (GDPR) in Europe, and similar regulations in other countries establish strict rules regarding the collection, storage, use, and disclosure of protected health information (PHI). These regulations mandate obtaining informed consent from patients before using their data, ensuring data security and minimizing the risk of data breaches. Adherence to these regulations is not merely a matter of compliance; it is essential for maintaining public trust and ensuring the ethical development and deployment of machine learning in healthcare. Non-compliance can lead to significant fines and legal repercussions. For instance, a healthcare provider failing to adequately secure patient data under HIPAA could face substantial penalties, impacting their reputation and financial stability. The GDPR, with its emphasis on data minimization and individual rights, sets a high bar for data protection, influencing regulatory approaches globally.
The Future of Machine Learning in Personalized Healthcare
The integration of machine learning (ML) into healthcare is still in its nascent stages, yet its potential to revolutionize how we prevent, diagnose, and treat diseases is undeniable. The coming years will witness an exponential growth in its applications, driven by both technological advancements and a growing understanding of its capabilities. This will lead to a healthcare system that is far more proactive, precise, and patient-centric.
Future applications will extend beyond current capabilities, moving from reactive interventions to proactive preventative measures. This shift will be fueled by increasingly sophisticated algorithms and the exponential growth of available data, leading to a more predictive and personalized approach to healthcare management.
Potential Future Applications of Machine Learning
The future of ML in personalized healthcare promises a wide range of applications, going far beyond current capabilities. We can anticipate advancements in areas like early disease detection through sophisticated image analysis and wearable sensor data interpretation. This will allow for interventions before symptoms even manifest, significantly improving patient outcomes. Furthermore, ML will play a crucial role in developing more effective and targeted therapies, minimizing side effects and maximizing treatment efficacy. Personalized medicine will become the norm, not the exception. For instance, imagine a future where your genetic makeup, lifestyle, and environmental factors are continuously monitored and analyzed to predict your risk of developing specific diseases years in advance, enabling timely preventative interventions.
Key Technological Advancements Shaping the Future
Several key technological advancements will propel the future of ML in personalized healthcare. First, advancements in computing power, particularly the rise of quantum computing, will allow for the processing of far larger and more complex datasets than is currently possible. This will unlock the potential of analyzing incredibly nuanced patient data, leading to more accurate and personalized insights. Second, the development of more robust and explainable AI models will address current concerns around the “black box” nature of some ML algorithms, increasing trust and transparency. Third, the integration of various data sources, including electronic health records (EHRs), genomics, wearable sensor data, and lifestyle information, will create a holistic view of the patient, enabling truly personalized interventions. Finally, improved data privacy and security measures will be crucial to ensure responsible and ethical use of this sensitive information.
A Futuristic Personalized Healthcare Scenario
Imagine a future where your personalized health assistant, powered by advanced ML, constantly monitors your vital signs through wearable sensors and analyzes your genetic predisposition to certain diseases. This assistant proactively identifies subtle changes indicative of potential health issues, alerting you and your physician well before symptoms appear. Based on this comprehensive analysis, your doctor can prescribe a precisely tailored treatment plan, including personalized medication dosages and lifestyle recommendations, all optimized for your unique genetic profile and health status. Regular check-ups become virtual consultations, with advanced imaging technologies analyzing your health in real-time, providing immediate feedback and eliminating the need for frequent in-person visits. This scenario isn’t science fiction; it’s a plausible future rapidly approaching, driven by the transformative power of machine learning in personalized healthcare. Consider, for example, the recent advancements in early cancer detection using AI-powered image analysis; this is a tangible example of the technology already improving patient outcomes and paving the way for even more sophisticated applications in the future.
Ending Remarks
The integration of machine learning into healthcare is no longer a futuristic fantasy; it’s rapidly becoming our reality. While challenges remain, the potential benefits—from earlier diagnoses and personalized treatments to accelerated drug discovery—are undeniable. As we move forward, responsible data handling and ethical considerations must be at the forefront. The future of healthcare is personalized, and machine learning is paving the way, one algorithm at a time. Get ready for a healthier, more precise tomorrow.
