The Future of Machine Learning in Personalized Healthcare is here, and it’s shaping up to be a game-changer. Imagine a world where your doctor has access to AI-powered tools that predict your risk for specific diseases, tailor treatments to your unique genetic makeup, and even monitor your health remotely through wearable sensors. This isn’t science fiction; it’s the rapidly evolving reality of personalized medicine, driven by the incredible power of machine learning.
This revolution isn’t without its challenges. Data privacy concerns are paramount, and integrating AI into existing healthcare systems requires careful planning and collaboration. But the potential benefits – earlier diagnoses, more effective treatments, and ultimately, healthier lives – are too significant to ignore. We’ll delve into the current applications, the ethical considerations, and the exciting innovations on the horizon.
Personalized Medicine: The Future Of Machine Learning In Personalized Healthcare
Personalized medicine, the tailoring of medical treatment to individual patients based on their unique genetic makeup, lifestyle, and environment, is rapidly evolving. While still in its nascent stages, it holds immense promise for revolutionizing healthcare, moving away from a “one-size-fits-all” approach to a more precise and effective model. However, significant hurdles remain before its widespread adoption.
Current State and Successes of Personalized Medicine
The current landscape of personalized medicine showcases both remarkable progress and significant limitations. Successes include the development of targeted cancer therapies, like Herceptin for HER2-positive breast cancer, which dramatically improved outcomes for specific patient populations. Pharmacogenomics, the study of how genes affect a person’s response to drugs, has also led to better drug selection and dosage adjustments, minimizing adverse effects. Genetic testing now routinely informs decisions regarding disease risk assessment and preventative measures, like BRCA gene testing for breast cancer risk. However, these successes are often limited to specific diseases and patient groups, leaving many underserved. The high cost of genetic testing and specialized therapies also creates accessibility issues, particularly for lower-income populations.
Ethical Considerations in Personalized Healthcare
The use of patient data in personalized healthcare raises complex ethical considerations. Data privacy and security are paramount concerns. Protecting sensitive genetic information from unauthorized access and misuse is crucial. Issues of informed consent also need careful consideration; patients must understand how their data will be used and have the right to control its access and use. The potential for genetic discrimination, where individuals are denied insurance or employment based on their genetic predispositions, is a significant ethical challenge requiring robust legal and regulatory frameworks. Equitable access to personalized medicine, ensuring that benefits aren’t concentrated among privileged groups, is another major ethical consideration.
Technological Barriers to Personalized Medicine Adoption
Several technological barriers hinder wider adoption of personalized medicine. The complexity of analyzing large genomic datasets requires advanced computational resources and sophisticated bioinformatics expertise, which are not readily available everywhere. Developing accurate and reliable predictive models for individual responses to treatments remains a challenge. Integration of diverse data sources, including genomic data, electronic health records, lifestyle information, and environmental factors, requires robust interoperability standards and data management systems. The lack of standardized protocols and guidelines for data sharing and analysis further complicates the development and implementation of personalized medicine approaches.
Comparison of Personalized Medicine Approaches
The following table compares different approaches to personalized medicine:
| Approach | Description | Advantages | Limitations |
|---|---|---|---|
| Pharmacogenomics | Tailoring drug therapy based on an individual’s genetic makeup. | Improved efficacy, reduced adverse drug reactions. | Limited availability of pharmacogenomic tests, complex interpretation of results. |
| Targeted Therapies | Developing drugs that specifically target cancer cells or other disease-causing agents. | Increased effectiveness, reduced side effects compared to traditional chemotherapy. | High cost, potential for drug resistance. |
| Lifestyle Interventions | Modifying lifestyle factors (diet, exercise, stress management) to improve health outcomes. | Cost-effective, reduces risk of chronic diseases. | Requires patient adherence, may not be suitable for all individuals. |
| Immunotherapy | Harnessing the body’s immune system to fight disease. | Effective against various cancers and other diseases. | High cost, potential for severe side effects. |
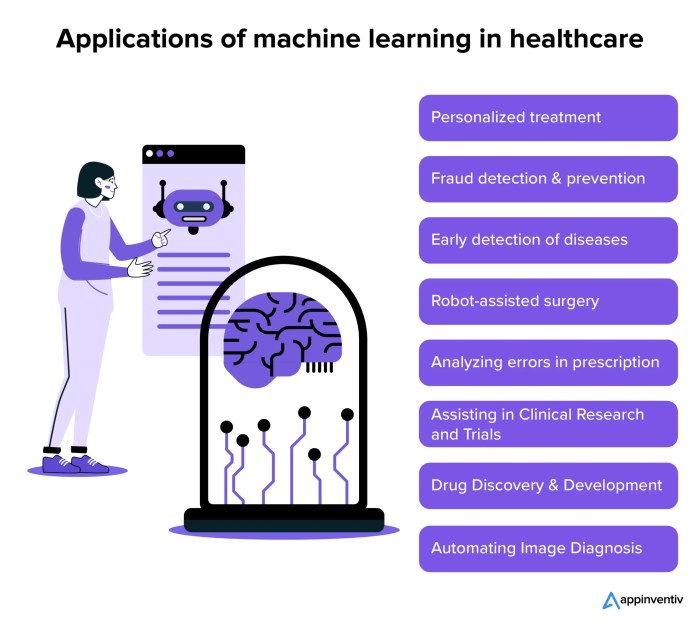
Machine Learning Applications in Personalized Healthcare

Source: solulab.com
Imagine a future where machine learning tailors healthcare to each individual, predicting risks and optimizing treatments. This personalized approach, however, needs global reach, and that’s where tech’s humanitarian role comes in; check out this insightful piece on The Role of Technology in Supporting Global Humanitarian Efforts to see how. Ultimately, expanding access to these advanced ML tools is key to ensuring equitable healthcare worldwide, creating a healthier future for all.
The integration of machine learning (ML) into healthcare is revolutionizing how we diagnose, treat, and manage diseases. It’s no longer a futuristic concept; ML algorithms are actively improving patient outcomes across various specialties, offering a level of personalization previously unimaginable. This section delves into specific applications and their impact.
Improved Diagnosis Through Machine Learning
Machine learning algorithms are proving incredibly adept at analyzing complex medical data – from medical images to genomic sequences – to aid in faster and more accurate diagnoses. For instance, in radiology, ML models trained on vast datasets of medical images (X-rays, CT scans, MRIs) can detect subtle anomalies often missed by the human eye, leading to earlier detection of cancers like lung cancer and breast cancer. Similarly, in pathology, ML assists in analyzing microscopic images of tissue samples to identify cancerous cells with greater precision and speed. These advancements not only improve diagnostic accuracy but also significantly reduce the time it takes to reach a diagnosis, enabling timely intervention and improved treatment outcomes. A study published in the *Journal of the American Medical Association* showed that an ML-based system achieved a higher accuracy rate in detecting diabetic retinopathy than experienced ophthalmologists, highlighting the potential for significant improvements in early detection and preventative care.
Machine Learning in Treatment Optimization and Patient Care
Beyond diagnosis, ML is transforming treatment planning and patient care. For example, in oncology, ML algorithms analyze patient data – including medical history, genetic information, and tumor characteristics – to predict treatment response and personalize chemotherapy regimens. This approach minimizes side effects while maximizing the effectiveness of treatment. In cardiology, ML models analyze electrocardiograms (ECGs) to identify individuals at high risk of heart failure, allowing for proactive interventions to prevent adverse events. Furthermore, ML-powered wearable sensors and mobile apps monitor patient vital signs and activity levels, providing real-time data to clinicians and enabling timely intervention should any abnormalities arise. This continuous monitoring improves patient engagement and allows for more proactive and personalized care. A successful example is the use of ML in predicting hospital readmissions, allowing healthcare providers to intervene and prevent unnecessary readmissions, improving patient outcomes and reducing healthcare costs.
AI’s Role in Personalized Drug Discovery and Development
The pharmaceutical industry is leveraging the power of AI and ML to accelerate drug discovery and development, leading to more targeted and effective personalized therapies. ML algorithms can analyze vast datasets of molecular structures and biological information to identify potential drug candidates, predict their efficacy and safety profiles, and optimize drug design. This significantly reduces the time and cost associated with traditional drug development, bringing personalized treatments to patients faster. For example, ML is being used to identify biomarkers that can predict which patients will respond best to a specific drug, allowing for more targeted therapies and reducing the risk of adverse drug reactions. Moreover, ML algorithms can analyze patient genomic data to identify individuals at high risk of developing specific diseases, paving the way for preventive therapies tailored to individual genetic predispositions.
Predicting Patient Risk: A Machine Learning Workflow
This flowchart depicts a simplified process of applying machine learning to predict patient risk. First, relevant patient data (medical history, genetic information, lifestyle factors) is collected and cleaned. Then, features are selected and engineered to create a suitable dataset for the ML model. A suitable model (e.g., logistic regression, random forest, support vector machine) is chosen and trained on the prepared data. After training, the model’s performance is evaluated using appropriate metrics. Finally, the model is deployed to predict the risk of a specific outcome (e.g., heart attack, stroke) for new patients. The entire process involves iterative refinement and validation to ensure accuracy and reliability.
Data Privacy and Security in Personalized Healthcare
Source: appinventiv.com
The promise of personalized medicine, fueled by machine learning, hinges on access to vast amounts of sensitive patient data. This creates a significant ethical and practical challenge: how do we leverage the power of this data to improve healthcare outcomes while simultaneously safeguarding individual privacy and security? The stakes are high; a breach of trust could severely undermine public confidence in this transformative technology.
The sheer volume and sensitivity of data involved in personalized healthcare present numerous vulnerabilities. From electronic health records (EHRs) containing genetic information, lifestyle details, and diagnoses, to wearable sensor data tracking real-time physiological parameters, the potential for misuse or unauthorized access is substantial. Furthermore, the integration of machine learning models, which often require extensive training datasets, amplifies these risks. Data breaches can lead to identity theft, discrimination, and reputational damage for both individuals and healthcare providers. Moreover, compromised data could be used to manipulate or bias algorithms, potentially leading to inaccurate diagnoses or inappropriate treatment recommendations.
Data Anonymization Techniques
Various techniques aim to protect patient privacy while still allowing for data analysis. These techniques attempt to remove or obscure identifying information, making it difficult to link data back to specific individuals. However, perfect anonymization is often elusive. Differentially private techniques add carefully calibrated noise to the data, making it difficult to extract precise information about individuals while preserving statistical properties. k-anonymity aims to ensure that each record is indistinguishable from at least k-1 other records based on a set of quasi-identifiers (e.g., age range, zip code). L-diversity adds a layer of protection by ensuring that sensitive attributes (e.g., diagnosis) have sufficient diversity within each k-anonymous group. Homomorphic encryption allows computations to be performed on encrypted data without decryption, protecting the underlying data even during analysis. The choice of technique depends on the specific context and the level of privacy required. For instance, a study analyzing population-level trends might employ a less stringent technique compared to a research project focusing on individual genetic predispositions.
Potential Vulnerabilities and Mitigation Strategies
Data breaches can occur at various points in the data lifecycle. Vulnerabilities exist in data storage, transmission, and processing. For example, poorly secured databases, inadequate access controls, and insecure APIs can all expose sensitive data to unauthorized access. Moreover, insider threats, such as malicious or negligent employees, pose a significant risk. Mitigation strategies include implementing robust security protocols, such as encryption, access control lists, and regular security audits. Data minimization—collecting only the necessary data—also reduces the risk of breaches. Employing multi-factor authentication and rigorous employee background checks can further enhance security. Regular penetration testing and vulnerability assessments can identify and address potential weaknesses before they can be exploited. Furthermore, robust incident response plans are crucial to minimize the impact of any successful breach.
Best Practices for Securing Sensitive Patient Data, The Future of Machine Learning in Personalized Healthcare
Protecting sensitive patient data used in machine learning models requires a multi-faceted approach. Simply put, robust security is paramount.
- Data Encryption: Encrypt data both at rest and in transit using strong encryption algorithms.
- Access Control: Implement strict access control measures, granting only authorized personnel access to sensitive data.
- Data Minimization: Collect only the minimum necessary data for the specific research or clinical application.
- Regular Security Audits: Conduct regular security audits and penetration testing to identify and address vulnerabilities.
- Secure Data Storage: Use secure storage solutions, such as cloud-based services with robust security features.
- Employee Training: Provide regular security awareness training to employees to prevent insider threats.
- Compliance with Regulations: Adhere to relevant data privacy regulations, such as HIPAA (in the US) and GDPR (in Europe).
- Differential Privacy Techniques: Incorporate differential privacy techniques into data analysis to protect individual privacy while preserving aggregate statistics.
- Federated Learning: Consider federated learning approaches that allow training machine learning models on decentralized data without directly sharing the data itself.
The Role of Big Data and Analytics
The convergence of personalized healthcare and advanced analytics is revolutionizing how we approach disease prevention, diagnosis, and treatment. Big data, with its massive datasets and complex algorithms, is no longer a futuristic concept; it’s the engine driving the precision medicine revolution. Unlocking the potential of this data is crucial for tailoring healthcare interventions to individual needs, leading to better outcomes and more efficient resource allocation.
Big data analytics significantly contributes to the development of personalized healthcare solutions by enabling the identification of patterns and insights that would be impossible to discern through traditional methods. By analyzing vast amounts of patient data, researchers and clinicians can develop more accurate risk prediction models, design more effective treatment strategies, and even predict individual responses to specific therapies. This level of personalization is transforming healthcare from a one-size-fits-all approach to a truly individualized experience.
Types of Data Used in Personalized Healthcare
Personalized healthcare relies on a diverse range of data sources to create a comprehensive picture of each patient’s health profile. These data types, when integrated effectively, provide a powerful foundation for developing personalized interventions.
The integration of genomic data, detailing an individual’s genetic makeup, is paramount. This allows for the identification of genetic predispositions to certain diseases, informing preventative measures and targeted therapies. Clinical data, encompassing medical history, diagnoses, treatments, and lab results, provides a chronological record of a patient’s health journey. Lifestyle data, including diet, exercise, sleep patterns, and environmental exposures, reveals crucial information about individual behaviors and their impact on health. Furthermore, wearable sensor data provides real-time insights into physiological parameters, enabling continuous monitoring and early detection of potential health issues. Finally, social determinants of health, such as socioeconomic status and access to healthcare resources, play a significant role in overall health outcomes and need to be considered.
Data Integration and Interoperability in Personalized Medicine
The true power of big data in personalized healthcare lies not just in the volume of data but in its integration and interoperability. Effectively combining genomic, clinical, lifestyle, and other data sources creates a holistic view of the patient, allowing for a more comprehensive and accurate assessment of their health status. However, this requires overcoming significant technical and logistical challenges. Different data sources often use different formats and standards, making it difficult to integrate them seamlessly. Interoperability, the ability of different systems to exchange and use data, is essential for overcoming these challenges. Standardized data formats, secure data exchange platforms, and robust data governance frameworks are critical for ensuring that data can be shared effectively across different healthcare providers and research institutions. Successful data integration allows for the development of more sophisticated predictive models, leading to improved diagnostic accuracy, more effective treatment strategies, and ultimately, better patient outcomes. For instance, integrating genomic data with clinical data might reveal that a patient with a specific genetic variant responds better to a particular medication, leading to a more targeted and effective treatment plan.
Advantages and Disadvantages of Different Data Sources
| Data Source | Advantages | Disadvantages | Examples |
|---|---|---|---|
| Genomic Data | Predictive power for disease risk, identification of drug targets, personalized treatment selection. | High cost, ethical concerns regarding data privacy and genetic discrimination, complex interpretation. | Genome-wide association studies (GWAS) identifying genes linked to specific diseases. |
| Clinical Data | Comprehensive record of patient’s health history, readily available in electronic health records (EHRs). | Inconsistent data quality, incomplete records, difficulty in standardizing across different systems. | Diagnosis codes, medication lists, lab results, imaging reports. |
| Lifestyle Data | Insights into patient behaviors influencing health, potential for early intervention and prevention. | Data collection can be challenging, self-reported data may be inaccurate or incomplete, privacy concerns. | Dietary habits, physical activity levels, sleep patterns, smoking status. |
| Wearable Sensor Data | Real-time physiological monitoring, early detection of health issues, continuous data collection. | Data accuracy can vary, potential for data overload, privacy concerns regarding continuous monitoring. | Heart rate, activity levels, sleep quality, blood glucose levels. |
Future Trends and Innovations
The convergence of machine learning (ML) and personalized healthcare is poised for explosive growth, driven by advancements in data acquisition, computational power, and our understanding of complex biological systems. This section explores emerging trends shaping the future of this exciting intersection, focusing on the transformative potential of AI and its integration with cutting-edge technologies.
The next generation of personalized healthcare will be characterized by a proactive, predictive, and preventative approach, moving beyond reactive treatment models. This shift is fueled by increasingly sophisticated AI algorithms capable of analyzing vast datasets to identify patterns, predict risks, and personalize interventions with unprecedented accuracy.
Predictive Diagnostics and Remote Patient Monitoring
AI’s ability to analyze medical images (like X-rays, CT scans, and MRIs) is rapidly improving diagnostic accuracy and speed. Algorithms are being trained on massive datasets of medical images, enabling them to detect subtle anomalies that might be missed by human clinicians. This is particularly impactful in areas like cancer detection, where early diagnosis significantly improves treatment outcomes. Simultaneously, remote patient monitoring (RPM) using wearable sensors and connected devices allows for continuous data collection, providing real-time insights into a patient’s health status. This continuous data stream, analyzed by AI algorithms, can trigger alerts for potential health deteriorations, enabling timely interventions and preventing hospital readmissions. For example, an AI-powered RPM system could monitor the heart rate and blood pressure of a patient with heart failure, alerting both the patient and their physician to any concerning changes.
The Role of Wearable Sensors and Other Technologies
Wearable sensors, including smartwatches, fitness trackers, and even implantable devices, are revolutionizing data collection in personalized healthcare. These devices continuously monitor various physiological parameters like heart rate, sleep patterns, activity levels, and even blood glucose levels. This rich stream of personalized data, combined with data from electronic health records (EHRs) and other sources, provides a comprehensive picture of an individual’s health status. The data gathered can be analyzed by AI algorithms to identify trends, predict potential health risks, and personalize treatment plans. For instance, a smartwatch detecting irregular heart rhythms could alert a patient and their doctor to the possibility of atrial fibrillation, allowing for prompt intervention and potentially preventing a stroke. Beyond wearables, other technologies like genomic sequencing and advanced imaging techniques contribute to the growing volume of personalized health data, further fueling the potential of AI-driven personalized healthcare.
A Hypothetical Future Scenario: AI-Managed Type 1 Diabetes
Imagine a future where managing type 1 diabetes is significantly less burdensome. An AI-powered system, integrated with a continuous glucose monitor (CGM) and an insulin pump, continuously monitors blood glucose levels and automatically adjusts insulin delivery based on individual needs and predicted trends. The system learns the patient’s unique metabolic responses to food, exercise, and stress, allowing for precise and personalized insulin adjustments, minimizing the risk of hypoglycemia and hyperglycemia. This AI-driven system also integrates with other health data sources, such as sleep patterns and activity levels, to provide a holistic view of the patient’s health and further refine insulin delivery. Furthermore, the system could predict potential complications, such as diabetic ketoacidosis, and alert the patient and their physician, enabling timely intervention. This hypothetical scenario highlights the potential of AI to significantly improve the quality of life for individuals with chronic conditions, reducing the burden of self-management and improving health outcomes. While this is a hypothetical scenario, many components already exist and are rapidly advancing toward this integrated approach.
Challenges and Opportunities
The integration of AI into healthcare, while promising a revolution in personalized medicine, isn’t without its hurdles. Existing systems, often built on legacy technology and siloed data, present significant challenges to seamless AI integration. Furthermore, the ethical considerations surrounding data privacy and algorithmic bias demand careful attention. However, the potential rewards – improved patient outcomes, reduced healthcare costs, and accelerated drug discovery – are immense, making the pursuit of these solutions a worthwhile endeavor.
Integrating AI into Existing Healthcare Systems
Successfully integrating AI-driven solutions into existing healthcare systems requires a multifaceted approach. The challenge lies not only in the technical aspects, such as data interoperability and system compatibility, but also in the organizational and cultural shifts needed within healthcare institutions. Many legacy systems lack the infrastructure to handle the vast amounts of data required for effective AI training and deployment. Furthermore, clinicians may be hesitant to adopt new technologies if they lack the necessary training and support. Overcoming these barriers requires a phased approach, starting with pilot projects in specific areas and gradually scaling up as confidence and expertise grow. Successful implementation will hinge on robust data governance frameworks, comprehensive staff training, and a commitment to continuous improvement.
Collaboration Between Stakeholders
The successful implementation of AI in personalized healthcare demands strong collaboration between healthcare providers, technology companies, and researchers. Healthcare providers possess the clinical expertise and patient data crucial for training and validating AI models. Technology companies bring the technical expertise in AI development and deployment. Researchers contribute to the advancement of AI algorithms and their application to specific healthcare challenges. Effective collaboration requires open communication channels, shared data governance frameworks, and a clear understanding of each stakeholder’s roles and responsibilities. Joint ventures, collaborative research projects, and industry consortia can foster this collaboration and accelerate innovation. For example, a partnership between a leading hospital, a tech giant specializing in machine learning, and a university research group could focus on developing an AI-powered diagnostic tool for a specific disease.
Strategies for Wider Adoption
Overcoming barriers to wider adoption requires a strategic approach focusing on several key areas. Firstly, investment in robust data infrastructure is crucial. This includes developing standardized data formats and interoperable systems that facilitate seamless data sharing across different healthcare settings. Secondly, comprehensive training and support programs for healthcare professionals are essential to ensure that they can effectively utilize AI-powered tools. Thirdly, addressing ethical concerns surrounding data privacy and algorithmic bias is paramount to building public trust and ensuring equitable access to AI-powered healthcare. Finally, regulatory frameworks need to be flexible and adaptive, encouraging innovation while maintaining appropriate safeguards to protect patient safety and privacy. For instance, the development of clear guidelines for AI algorithm validation and deployment could accelerate the adoption of trustworthy AI systems.
Policy Recommendations for Fostering Innovation
To foster innovation in personalized healthcare, policymakers should consider the following recommendations:
- Invest in research and development of AI technologies for healthcare.
- Establish clear ethical guidelines and regulatory frameworks for the use of AI in healthcare.
- Promote data sharing and interoperability across healthcare systems.
- Support the development of training programs for healthcare professionals on the use of AI.
- Incentivize the development and adoption of AI-powered healthcare solutions.
- Foster collaboration between healthcare providers, technology companies, and researchers.
- Establish mechanisms for monitoring and evaluating the effectiveness and safety of AI-powered healthcare solutions.
Wrap-Up
The convergence of machine learning and personalized healthcare promises a future where medicine is proactive, predictive, and profoundly personalized. While hurdles remain – from data security to system integration – the potential to transform healthcare is undeniable. By addressing ethical concerns and fostering collaboration, we can unlock the transformative power of AI to improve the lives of millions. The future of health is intelligent, and it’s here.
