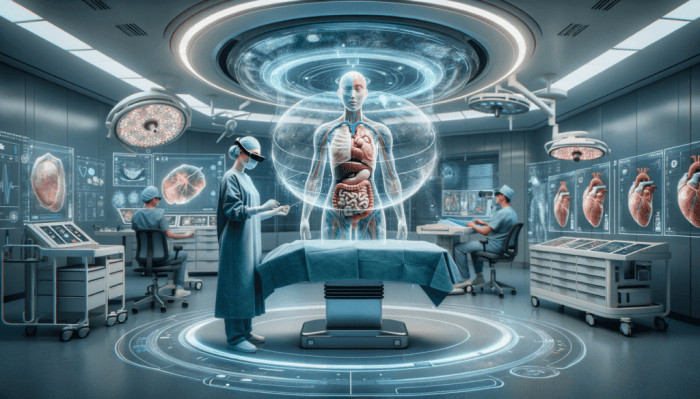
The Future of Augmented Reality in Healthcare for Enhanced Patient Care is no longer science fiction; it’s rapidly becoming our reality. Imagine surgeons wielding tools guided by holographic overlays, medical students practicing complex procedures in immersive simulations, and patients recovering faster thanks to engaging AR-powered therapies. This isn’t just about cool tech; it’s about a revolution in how we deliver and receive healthcare, boosting precision, accessibility, and ultimately, patient outcomes.
From minimally invasive surgeries guided by AR overlays to remote consultations using smart glasses, the applications are vast and rapidly evolving. The integration of AI and 5G promises even more seamless and effective solutions, paving the way for personalized medicine and proactive health management. But this technological leap isn’t without its hurdles; data privacy, cost-effectiveness, and ethical considerations are key challenges that need careful navigation.
Current Applications of AR in Healthcare
Source: gravityjack.com
Augmented reality (AR) is rapidly transforming healthcare, moving beyond the realm of science fiction and into the everyday practice of medicine. By overlaying digital information onto the real world, AR enhances precision, improves training, and personalizes patient care in ways previously unimaginable. This section explores several key areas where AR is already making a significant impact.
Augmented Reality in Surgical Procedures
AR is revolutionizing surgical procedures by providing surgeons with real-time, three-dimensional visualizations of a patient’s anatomy. This allows for greater precision during complex operations, minimizing invasiveness and improving patient outcomes. For instance, during minimally invasive cardiac surgery, AR overlays a 3D model of the patient’s heart onto the surgeon’s view, guiding the placement of catheters and other instruments with millimeter accuracy. Similarly, in neurosurgery, AR can project a patient’s brain scan onto the surgical field, allowing surgeons to navigate complex anatomical structures with greater confidence and reduce the risk of unintended damage to healthy tissue. The improved visualization leads to smaller incisions, reduced trauma, shorter recovery times, and ultimately, better patient experiences.
Augmented Reality in Medical Training and Education
AR offers a powerful tool for medical training and education, allowing students and professionals to practice complex procedures in a safe and controlled environment. AR simulations provide realistic scenarios that mimic real-world surgical challenges, enabling trainees to develop their skills and refine their techniques without the risks associated with live surgery. For example, medical students can use AR headsets to practice laparoscopic surgery, receiving immediate feedback on their technique and identifying areas for improvement. These simulations can be customized to represent a variety of patient anatomies and surgical scenarios, providing a more comprehensive and engaging learning experience than traditional methods. Furthermore, AR can be used to visualize complex anatomical structures in 3D, enhancing understanding and retention of information.
Augmented Reality in Patient Rehabilitation and Physical Therapy
AR is proving to be invaluable in patient rehabilitation and physical therapy, providing engaging and personalized treatment plans. By gamifying the rehabilitation process, AR applications can motivate patients to actively participate in their recovery, leading to improved outcomes. Consider a hypothetical AR application for stroke rehabilitation: the application would project interactive games onto a screen or a table in front of the patient. These games would require the patient to perform specific exercises, such as reaching for virtual objects or tracing patterns with their affected limb. The application would track the patient’s movements, providing real-time feedback on their performance and adjusting the difficulty level as they progress. The gamified nature of the application would keep patients engaged and motivated, while the personalized feedback would ensure that they are working at the appropriate intensity. This combination of engagement and personalized feedback would lead to better adherence to the rehabilitation program and ultimately faster recovery.
Comparison of AR-Assisted Therapy vs. Traditional Methods for Post-Surgical Recovery
The following table compares the effectiveness of AR-assisted therapy versus traditional methods for post-surgical knee replacement recovery. While further large-scale studies are needed to definitively establish superiority, early indications suggest significant potential benefits from AR.
| Factor | AR-Assisted Therapy | Traditional Therapy | Notes |
|---|---|---|---|
| Patient Engagement | High; gamified exercises increase motivation. | Moderate; relies on patient compliance. | AR’s interactive nature can improve adherence to exercise routines. |
| Progress Tracking | Real-time data on range of motion, strength, etc. | Manual measurements, subjective assessments. | AR provides objective data for more accurate progress monitoring. |
| Recovery Time | Potentially faster due to increased engagement and personalized feedback. | Variable, depending on patient and therapy adherence. | Studies show promise, but further research is required to confirm. |
| Cost-Effectiveness | Initial investment in technology; long-term cost-effectiveness needs further evaluation. | Lower initial cost; but potential for longer recovery times and increased healthcare utilization. | A cost-benefit analysis comparing the two approaches is necessary. |
Future Trends in AR Healthcare Technology
Augmented reality (AR) is poised to revolutionize healthcare, moving beyond its current applications to integrate seamlessly into various aspects of patient care. The future of AR in healthcare promises a more personalized, efficient, and accessible system, leveraging advancements in technology to improve both patient outcomes and the efficiency of healthcare delivery. This section explores the key trends shaping this exciting evolution.
Remote Patient Monitoring and Telehealth Enhanced by AR
AR’s potential in remote patient monitoring and telehealth is immense. Imagine a patient recovering from surgery at home, wearing smart glasses that allow a doctor to remotely view their incision, check for signs of infection, and provide real-time guidance on wound care. This eliminates the need for frequent in-person visits, reduces hospital readmissions, and improves patient adherence to post-operative instructions. Furthermore, AR can enhance patient engagement by overlaying interactive 3D models of their anatomy onto their body, allowing them to better understand their condition and treatment plan. For example, a patient with diabetes could use an AR app to visualize the impact of different food choices on their blood sugar levels, promoting better self-management. The use of AR in remote consultations also allows for more effective communication, with doctors able to annotate images, highlight areas of concern, and even virtually manipulate medical equipment during the consultation.
Emerging Technologies Shaping the Future of AR in Healthcare
Several emerging technologies will significantly impact the future of AR in healthcare. 5G connectivity, with its high speed and low latency, will be crucial for enabling real-time data transmission from AR devices to healthcare professionals. This is particularly important for remote surgery or consultations where even a slight delay could have significant consequences. Imagine a surgeon performing a minimally invasive procedure guided by high-resolution AR overlays provided in real-time through a 5G connection. The integration of artificial intelligence (AI) with AR is another key development. AI algorithms can analyze data collected from AR devices, providing clinicians with valuable insights into patient health, such as early detection of anomalies or personalized treatment recommendations. For example, AI could analyze images captured by an AR headset during a neurological exam to detect subtle signs of a stroke, potentially leading to faster intervention and improved patient outcomes. The combination of 5G and AI creates a powerful synergy, allowing for faster, more accurate, and more personalized healthcare.
Comparison of AR Hardware for Healthcare Applications
The choice of AR hardware depends on the specific healthcare application. Several devices are suitable for various purposes.
- Smart Glasses: Advantages include hands-free operation, allowing clinicians to access patient data and medical images without interrupting their workflow. Disadvantages include limited field of view and processing power, potentially restricting the complexity of AR overlays. Examples include Google Glass Enterprise Edition and Microsoft HoloLens 2.
- Headsets: Advantages include immersive experiences and high-resolution displays, ideal for complex surgical procedures or medical training simulations. Disadvantages include higher cost, bulkier design, and potential for motion sickness. Examples include the Oculus Rift and HTC Vive.
- Mobile Devices (Tablets and Smartphones): Advantages include widespread availability, affordability, and ease of use. Disadvantages include limited hands-free capabilities and less immersive experience compared to headsets or smart glasses. Examples include iPads and various Android tablets.
Hypothetical Scenario: AR and Wearable Sensors for Continuous Patient Monitoring, The Future of Augmented Reality in Healthcare for Enhanced Patient Care
Imagine a patient with congestive heart failure wearing a smartwatch equipped with multiple sensors that continuously monitor heart rate, blood pressure, oxygen saturation, and activity levels. This data is transmitted wirelessly to a cloud-based platform where an AI algorithm analyzes it in real-time. An AR application on the patient’s smartphone or tablet displays this data in a visually intuitive manner, providing personalized feedback and alerts. For example, if the patient’s heart rate rises above a pre-defined threshold, the AR application could display a warning message and suggest appropriate actions, such as resting or contacting their physician. The AI algorithm could also identify patterns indicative of worsening heart failure, enabling proactive intervention and preventing hospitalizations. The collected data can also be used to personalize treatment plans, adjusting medication dosages or recommending lifestyle changes based on the patient’s individual response. This continuous monitoring system, enabled by the integration of AR and wearable sensors, could significantly improve the management of chronic conditions and enhance patient outcomes.
Challenges and Opportunities in AR Adoption: The Future Of Augmented Reality In Healthcare For Enhanced Patient Care
Augmented reality’s potential in healthcare is undeniable, but its widespread adoption faces significant hurdles. Successfully integrating AR requires navigating complex issues related to data security, cost-effectiveness, regulatory compliance, and user experience. Addressing these challenges is crucial to unlocking AR’s transformative power in patient care.
Data Privacy and Security Concerns in AR-Based Healthcare
The use of AR in healthcare necessitates the collection and processing of sensitive patient data, raising significant privacy and security concerns. AR applications often require access to medical images, patient records, and real-time physiological data, making them attractive targets for cyberattacks. Breaches could lead to identity theft, medical misinformation, and compromised patient trust. Robust security measures, including data encryption, secure cloud storage, and rigorous access control protocols, are essential. Furthermore, adhering to regulations like HIPAA in the US and GDPR in Europe is paramount. Implementing multi-factor authentication, regular security audits, and employee training on data protection best practices are vital steps in mitigating these risks. The development of privacy-preserving technologies, such as federated learning and differential privacy, can also help minimize data exposure while still enabling valuable analysis and model training.
Cost Implications of Implementing AR Technologies in Healthcare
The initial investment in AR technology can be substantial, encompassing hardware costs (AR headsets, sensors, etc.), software development, training for healthcare professionals, and ongoing maintenance. The cost per patient can also be significant, particularly with specialized AR applications requiring expensive equipment or highly trained personnel. However, the long-term cost-effectiveness of AR needs careful consideration. Strategies to mitigate costs include leveraging cloud-based solutions to reduce hardware costs, focusing on AR applications with a high return on investment (ROI), and exploring public-private partnerships to share the financial burden. Furthermore, demonstrating a clear clinical benefit and improved patient outcomes through rigorous clinical trials can justify the investment to healthcare providers and payers. For example, a hospital system could pilot an AR-based surgical training program in a limited capacity, demonstrating its effectiveness before scaling it across the entire organization.
Regulatory Hurdles and Ethical Considerations in AR Healthcare
The deployment of AR in healthcare faces regulatory challenges related to device approval, data privacy, and clinical validation. Ethical considerations include ensuring patient autonomy, avoiding bias in algorithms, and addressing potential risks associated with the technology’s use. A robust framework for ethical guidelines is needed to ensure responsible innovation. This framework should include clear principles for data privacy, informed consent, algorithmic transparency, and risk mitigation. Regular audits and independent review boards should be established to oversee the development and deployment of AR applications. For instance, guidelines should specify the criteria for determining when AR applications are ready for clinical use, including rigorous testing and validation to ensure safety and efficacy. Clear procedures for reporting adverse events and addressing potential biases in algorithms are also crucial components of such a framework.
The Importance of User Experience (UX) Design in AR Healthcare Applications
Intuitive and user-friendly UX design is paramount for successful AR adoption in healthcare. Poorly designed applications can lead to frustration, reduced patient compliance, and ultimately, failure to achieve the intended clinical benefits.
- Intuitive Interfaces: AR applications should feature simple, clear, and easily navigable interfaces. Avoid complex menus and jargon; prioritize visual clarity and ease of use. For example, a patient rehabilitation app could use simple visual cues and gamification elements to guide patients through exercises, rather than relying on complex textual instructions.
- Personalized Experiences: Tailoring AR experiences to individual patient needs and preferences can significantly improve engagement and compliance. For example, a diabetes management app could personalize reminders and educational content based on a patient’s specific needs and progress.
- Accessibility and Inclusivity: AR applications should be designed to be accessible to patients with diverse needs and abilities, including those with visual or cognitive impairments. For example, using audio cues and haptic feedback in addition to visual displays can make the application more inclusive.
- Feedback Mechanisms: Integrating feedback mechanisms allows for continuous improvement of the AR application based on user input. This could include surveys, in-app feedback forms, or usability testing sessions.
Impact on Patient Care and Outcomes
Augmented reality (AR) is poised to revolutionize healthcare, significantly impacting patient care and ultimately leading to better outcomes. By overlaying digital information onto the real world, AR offers a range of benefits that improve diagnosis, treatment, patient engagement, and overall experience, ultimately leading to cost savings within the healthcare system.
AR’s impact on patient care extends beyond simple visualization; it facilitates a more precise and personalized approach to healthcare, improving both the efficiency and effectiveness of treatment.
Augmented reality’s potential in healthcare is huge, imagine surgeons with real-time data overlays during procedures! This level of personalized assistance is only going to get better as AI develops, much like the advancements we’re seeing in personal assistants, as highlighted in this article on How AI is Transforming the World of Personal Assistants. Ultimately, this AI-driven precision will lead to even more effective and efficient AR tools for patient care, revolutionizing diagnostics and treatment.
Improved Diagnostic Accuracy and Treatment Planning
AR can dramatically improve the accuracy of diagnoses and the effectiveness of treatment plans. For instance, surgeons can use AR headsets to visualize a patient’s internal anatomy during surgery, overlaid with real-time data from medical imaging like CT scans or MRIs. This allows for more precise incisions and reduces the risk of complications. Similarly, radiologists can use AR to review medical images in 3D, making it easier to identify subtle anomalies that might be missed in traditional 2D views. Imagine a cardiologist using AR glasses to pinpoint the exact location of a blockage in a coronary artery during a minimally invasive procedure – this level of precision directly translates to better patient outcomes. Another example would be orthopedic surgeons using AR overlays during joint replacement surgeries to ensure perfect implant placement.
Enhanced Patient Engagement and Treatment Adherence
AR technology can significantly boost patient engagement and improve adherence to prescribed treatment regimens. Consider a hypothetical case: Sarah, a diabetic patient, struggles to manage her blood sugar levels effectively. Using an AR application on her smartphone, Sarah can scan her food to get instant nutritional information, receive personalized reminders to take her medication, and visualize the impact of her dietary choices on her blood sugar levels in real-time through interactive 3D models. This interactive, personalized approach makes managing her diabetes less daunting and more manageable, leading to better adherence and improved health outcomes. AR-based games can also gamify rehabilitation exercises, motivating patients to consistently complete their therapy.
Impact on Patient Satisfaction and Quality of Life
AR has the potential to significantly improve patient satisfaction and quality of life. For example, AR apps can guide patients through complex medical procedures at home, reducing anxiety and improving their understanding of their condition. Imagine a patient recovering from knee surgery using an AR app to visualize and follow their physiotherapy exercises accurately, boosting their confidence and speeding up their recovery. AR can also be used to create immersive virtual reality environments for pain management, distracting patients from discomfort and promoting relaxation. The ability to visualize their own medical data in an easily understandable format empowers patients, fostering a sense of control and participation in their healthcare journey.
Reduction in Healthcare Costs
AR can contribute to substantial cost savings in healthcare by improving efficiency and reducing medical errors.
| Cost Reduction Strategy | Mechanism | Example | Estimated Savings |
|---|---|---|---|
| Improved Surgical Precision | Reduced operative time, fewer complications | AR-guided surgery leading to shorter hospital stays and reduced need for revision surgeries | Potentially significant reduction in hospital costs and post-operative care expenses. |
| Enhanced Medical Training | Reduced training time, improved skill acquisition | AR simulations for medical students and surgeons leading to quicker competency development | Lower training costs, higher efficiency of healthcare professionals. |
| Improved Diagnostic Accuracy | Reduced misdiagnosis, fewer unnecessary tests | AR-assisted radiology leading to more accurate identification of diseases, avoiding costly and invasive procedures | Lower costs associated with unnecessary tests and procedures. |
| Increased Patient Engagement | Improved treatment adherence, reduced hospital readmissions | AR-based patient education and remote monitoring leading to better self-management and fewer hospital visits | Lower healthcare utilization costs, reduced burden on healthcare systems. |
Specific AR Applications in Different Medical Specialties

Source: cifs.health
Augmented reality (AR) is rapidly transforming healthcare, offering innovative solutions across various medical specialties. Its ability to overlay digital information onto the real world provides surgeons with enhanced visualization, aids radiologists in image interpretation, and assists specialists in diagnosis and treatment planning. This section explores specific AR applications in surgery, radiology, ophthalmology, and dermatology, highlighting their unique benefits and potential to revolutionize patient care.
AR in Surgery
AR applications in surgery are enhancing precision and minimizing invasiveness. In neurosurgery, for example, AR systems can overlay 3D models of a patient’s brain anatomy onto the surgical field, guiding the surgeon with real-time data during complex procedures. This improves accuracy in tumor removal and reduces the risk of damaging critical brain structures. Similarly, in orthopedics, AR can guide the placement of implants, ensuring accurate positioning and minimizing the need for extensive surgical intervention. The benefits include reduced surgical time, improved accuracy, and faster patient recovery.
AR in Radiology and Medical Imaging
AR is revolutionizing the way radiologists interpret medical images. AR interfaces can overlay relevant patient data, such as medical history and previous scans, directly onto the images. This allows for a more comprehensive understanding of the patient’s condition, aiding in faster and more accurate diagnosis. Furthermore, AR can enable interactive 3D visualizations of complex anatomical structures, providing radiologists with a more intuitive and insightful view of the images. This leads to improved diagnostic accuracy and potentially reduces the need for additional imaging tests.
AR in Ophthalmology and Dermatology
In ophthalmology, AR applications are being used to assist in retinal surgery and diagnosis. AR headsets can overlay real-time data onto the surgeon’s view, providing precise guidance during complex procedures. For instance, AR can help in the accurate placement of retinal implants or guide the surgeon during vitrectomy. In dermatology, AR apps can help analyze skin lesions, compare them to a database of known conditions, and provide a preliminary diagnosis. This can aid dermatologists in identifying potentially cancerous lesions and ensuring timely treatment. Patients can also use AR apps to monitor their skin conditions and track changes over time.
AR Application in Cardiology: A Visual Representation
Imagine a cardiologist wearing AR glasses during a cardiac catheterization procedure. The glasses overlay a real-time 3D model of the patient’s heart and blood vessels onto the live fluoroscopy feed. The model is generated from the patient’s pre-procedure CT scan. Key features include: real-time anatomical data, highlighting of critical structures (valves, arteries), and a virtual guide wire showing the optimal path for catheter insertion. This allows the cardiologist to visualize the procedure in 3D, improving precision and reducing the risk of complications. The patient benefits from a potentially less invasive procedure, faster recovery time, and improved overall outcomes. The cardiologist benefits from enhanced visualization, reduced procedure time, and increased precision, leading to better patient care.
Conclusive Thoughts
The integration of augmented reality into healthcare is poised to redefine patient care, ushering in an era of precision, personalization, and accessibility. While challenges remain, the potential benefits—from improved surgical outcomes and streamlined medical training to enhanced patient engagement and reduced healthcare costs—are undeniable. The future of healthcare is augmented, and the journey is only just beginning. The next decade will witness breathtaking advancements, transforming not just how we treat illness, but how we proactively maintain health and well-being.
