How Machine Learning Algorithms Are Improving Healthcare Outcomes? It’s a question that’s rapidly moving from futuristic fantasy to everyday reality. From dramatically speeding up diagnoses and personalizing treatments to revolutionizing drug discovery and streamlining hospital operations, machine learning is quietly reshaping the healthcare landscape. This isn’t just about efficiency; it’s about fundamentally improving patient care and outcomes, tackling disparities, and even pushing the boundaries of what’s medically possible.
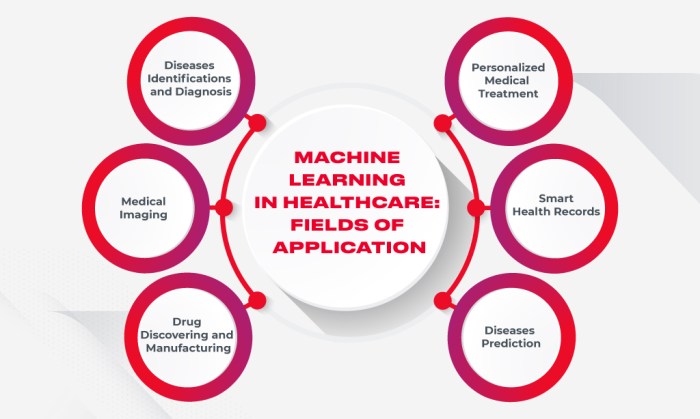
This deep dive explores the multifaceted ways machine learning is transforming healthcare. We’ll examine how algorithms analyze medical images with incredible accuracy, predict disease progression, personalize treatment plans, and even accelerate the development of life-saving drugs. We’ll also discuss the ethical considerations and challenges that come with this powerful technology, ensuring a balanced and insightful perspective on this rapidly evolving field.
Improved Diagnostics
Machine learning (ML) is revolutionizing healthcare, particularly in diagnostics. Its ability to analyze vast amounts of data quickly and accurately is transforming how we detect and diagnose diseases, leading to better patient outcomes and more efficient healthcare systems. This enhanced diagnostic capability stems from ML algorithms’ prowess in pattern recognition and prediction, surpassing traditional methods in speed, accuracy, and cost-effectiveness.
ML algorithms are significantly enhancing the accuracy and speed of medical image analysis. Traditional methods rely heavily on human expertise, which can be subjective and time-consuming. ML, on the other hand, can analyze medical images like X-rays, CT scans, and MRIs much faster and often more accurately than human radiologists, particularly in identifying subtle anomalies that might be missed by the human eye.
Medical Image Analysis: Traditional vs. ML-Powered Methods
The following table compares traditional methods with ML-powered methods in medical image analysis, highlighting the advantages of ML in speed, accuracy, and cost-effectiveness.
| Feature | Traditional Methods | ML-Powered Methods |
|---|---|---|
| Speed | Slow, often requiring hours or days for analysis, depending on image complexity and radiologist availability. | Fast, capable of analyzing images in seconds or minutes, enabling rapid diagnosis and treatment. |
| Accuracy | Can be subjective and prone to human error; inter-observer variability can be significant. | Higher accuracy, especially in detecting subtle anomalies; reduces inter-observer variability. Accuracy often surpasses human performance in specific tasks. |
| Cost-Effectiveness | High labor costs, particularly with specialist radiologists. Potential for delays leading to increased hospital stays and treatment costs. | Potentially lower long-term costs due to faster diagnosis, reduced need for repeated scans, and improved treatment efficiency. Initial investment in ML infrastructure is required. |
Early Disease Detection with Machine Learning
ML’s ability to identify patterns in large datasets is proving invaluable in early disease detection. This early detection often translates to better treatment outcomes and improved survival rates. Specific examples include cancer screening and cardiovascular risk assessment.
In cancer screening, ML algorithms can analyze mammograms to detect subtle signs of breast cancer, often earlier than traditional methods. Similarly, ML is being used to analyze CT scans to detect lung cancer nodules, improving the accuracy and efficiency of lung cancer screening programs. For cardiovascular risk assessment, ML algorithms can analyze patient data, including medical history, lifestyle factors, and genetic information, to predict the likelihood of developing cardiovascular disease, allowing for preventative measures to be implemented early.
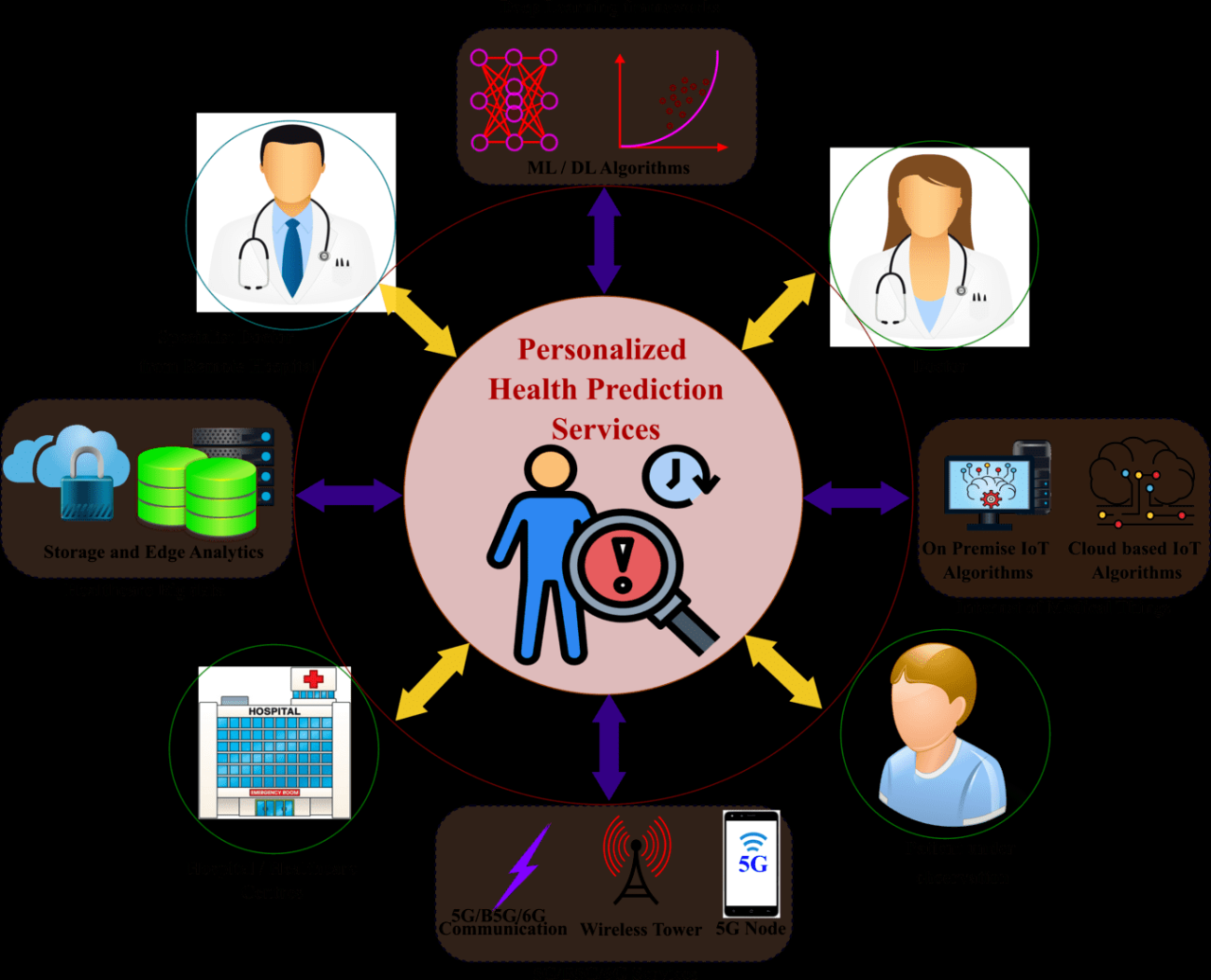
Analyzing Patient Data for Disease Prediction
Machine learning algorithms are increasingly used to analyze electronic health records (EHRs) and other patient data to identify patterns and predict disease progression. By analyzing large datasets of patient information, ML can identify risk factors and predict the likelihood of developing specific diseases, enabling proactive interventions and personalized treatment plans.
For instance, ML models can predict the risk of hospital readmission after a heart attack, allowing healthcare providers to take proactive steps to prevent readmission. Similarly, ML can predict the progression of chronic diseases like diabetes and kidney disease, allowing for timely adjustments to treatment plans and improved patient management. The ability to predict disease progression empowers healthcare providers to make more informed decisions and improve overall patient care.
Personalized Treatment Plans
Source: innovecs.com
The era of one-size-fits-all medicine is fading fast. Machine learning is revolutionizing healthcare by enabling the creation of highly personalized treatment plans, tailored to the unique characteristics of each individual patient. This approach moves beyond broad treatment guidelines, offering a more precise and effective path to recovery.
Machine learning algorithms analyze vast datasets encompassing genetics, lifestyle factors, medical history, and real-time patient data to predict treatment response and optimize treatment strategies. This personalized approach promises to significantly improve patient outcomes, reduce adverse effects, and enhance overall healthcare efficiency.
Tailoring Treatment to Individual Characteristics
Machine learning algorithms excel at identifying patterns and correlations within complex datasets. In personalized treatment planning, these algorithms analyze a patient’s genetic makeup (including pharmacogenomics, which studies how genes affect a person’s response to drugs), lifestyle choices (diet, exercise, smoking), medical history (previous treatments, diagnoses, allergies), and current health status to create a customized treatment strategy. For example, an algorithm might identify a genetic predisposition to a specific side effect of a particular drug, prompting a physician to select an alternative medication with a lower risk profile for that individual. Similarly, lifestyle factors such as diet and exercise can influence the effectiveness of certain treatments, and machine learning can help integrate this information into treatment planning.
Optimizing Drug Dosages and Treatment Schedules
One of the key benefits of machine learning in personalized medicine is the ability to optimize drug dosages and treatment schedules. Traditional approaches often involve a trial-and-error method, potentially leading to suboptimal therapeutic effects or harmful side effects. Machine learning algorithms, however, can predict an individual’s optimal drug dose and treatment frequency based on their unique characteristics and response to treatment. This predictive capability minimizes the risk of adverse events and maximizes the therapeutic benefit, leading to better patient outcomes. For instance, in cancer treatment, algorithms can predict a patient’s response to chemotherapy based on their tumor’s genetic profile, allowing oncologists to tailor the dosage and schedule to maximize efficacy while minimizing toxicity.
Successful Applications of Machine Learning in Personalized Medicine
Machine learning has already demonstrated its potential in several areas of personalized medicine. In oncology, algorithms are used to predict cancer risk, diagnose different cancer types, and personalize treatment plans based on tumor genetics and patient characteristics. For example, algorithms are being used to predict which patients with breast cancer are most likely to benefit from chemotherapy, thus avoiding unnecessary treatment and its associated side effects. In cardiology, machine learning helps predict the risk of heart attacks and strokes, allowing for early intervention and preventative measures. Similarly, in diabetes management, algorithms personalize insulin dosages based on continuous glucose monitoring data, leading to better glycemic control and reduced complications. The development of personalized medicine through machine learning is rapidly expanding, impacting a growing number of diseases and treatment areas.
Enhanced Drug Discovery and Development
The pharmaceutical industry, traditionally a slow-moving behemoth, is undergoing a radical transformation thanks to the power of machine learning. This isn’t just about speeding things up; it’s about fundamentally changing how we discover, develop, and deliver life-saving medications. Machine learning algorithms are proving invaluable in navigating the complexities of drug discovery and development, offering a level of precision and efficiency previously unimaginable.
Machine learning accelerates drug discovery by analyzing massive datasets to identify potential drug candidates and predict their efficacy. This involves sifting through millions of molecular structures, identifying those most likely to bind to specific targets involved in diseases, and predicting their effectiveness and potential side effects. This significantly reduces the time and cost associated with traditional trial-and-error methods. For example, Atomwise, a company utilizing AI, successfully identified two potential Ebola treatments in a matter of days, a feat that would have taken years using traditional methods.
Machine Learning in Drug Candidate Identification and Efficacy Prediction
The application of machine learning in this area is multifaceted. Algorithms can analyze genomic data to identify potential drug targets, predict the effectiveness of drug candidates based on their molecular structure and properties, and even design entirely new molecules with desired characteristics. This allows researchers to focus their efforts on the most promising candidates, reducing the risk of investing time and resources in compounds that are unlikely to succeed. Imagine a scenario where an algorithm can predict with 90% accuracy whether a molecule will be effective against a specific cancer type – that’s the potential we’re talking about. This predictive power allows for a more targeted and efficient drug development pipeline.
Analyzing Clinical Trial Data with Machine Learning
Clinical trials are notoriously expensive and time-consuming. Machine learning offers a powerful tool to analyze the vast amounts of data generated during these trials, identifying effective treatments, predicting patient responses, and even optimizing trial design. For instance, machine learning can identify subtle patterns in patient data that might indicate which patients are most likely to respond to a particular treatment, leading to more personalized and effective therapies. By predicting treatment efficacy in advance, researchers can make better decisions about which treatments to pursue and potentially avoid investing in treatments that are unlikely to succeed in a larger population. This analysis can help identify potential adverse events earlier and more effectively than traditional methods.
Traditional vs. Machine Learning-Driven Drug Development
Traditional drug development relies heavily on trial and error, involving extensive laboratory testing and clinical trials. This approach is time-consuming, expensive, and has a high failure rate. In contrast, machine learning-driven approaches leverage computational power to analyze vast datasets, identifying promising candidates and predicting their efficacy more efficiently. The table below summarizes the key differences:
| Feature | Traditional Methods | Machine Learning-Driven Methods |
|---|---|---|
| Candidate Identification | Trial and error, based on chemical intuition and biological knowledge | High-throughput screening, computational modeling, and analysis of large datasets |
| Efficacy Prediction | In-vivo and in-vitro testing, preclinical studies | Predictive modeling based on molecular properties, genomic data, and clinical trial data |
| Time to Market | 10-15 years | Potentially significantly reduced |
| Cost | Billions of dollars | Potentially significantly reduced |
| Success Rate | Low (approximately 10%) | Potentially increased |
Advantages and Disadvantages of Machine Learning in Drug Development
It’s crucial to acknowledge both the potential and limitations of machine learning in this field.
The advantages are significant: increased speed and efficiency, reduced costs, improved accuracy in prediction, and the potential for personalized medicine. However, there are also disadvantages: the need for high-quality data, the risk of bias in algorithms, the “black box” nature of some models making it difficult to understand their decision-making process, and the ethical considerations surrounding the use of patient data. These challenges require careful consideration and ongoing research to ensure responsible and effective implementation of machine learning in drug development.
Improved Operational Efficiency in Healthcare
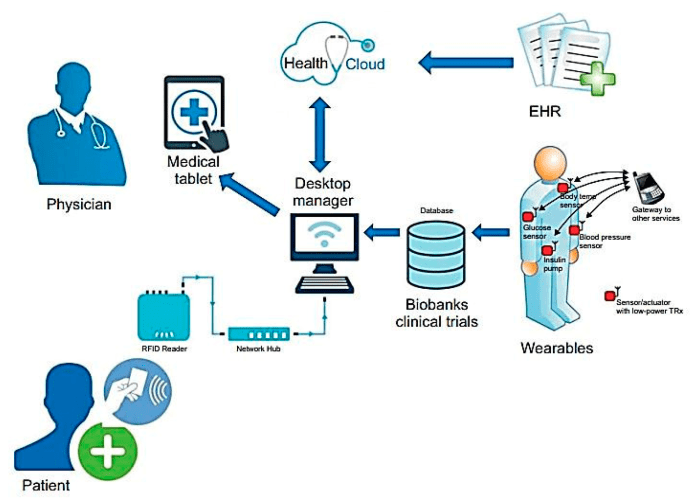
Source: mdpi.com
Machine learning is quietly revolutionizing healthcare, not just in flashy breakthroughs like personalized medicine, but also in the often-overlooked realm of operational efficiency. By crunching vast amounts of data – patient records, staffing schedules, equipment maintenance logs – ML algorithms are streamlining processes, saving money, and ultimately, improving patient care. This isn’t about robots replacing doctors; it’s about empowering healthcare professionals with smarter tools to do their jobs better.
The impact of machine learning on hospital operations is significant, leading to better resource allocation, reduced wait times, and improved equipment reliability. This translates to happier staff, more satisfied patients, and a healthier bottom line for healthcare providers. Let’s delve into some specific examples.
Optimized Resource Allocation
Efficient resource allocation is the cornerstone of any well-functioning hospital. Machine learning algorithms excel at analyzing complex datasets to predict future needs and optimize the use of limited resources. This includes everything from bed management to staff scheduling, leading to significant cost savings and improved patient care.
- Predictive Bed Management: ML models can analyze historical data (patient admissions, lengths of stay, discharge rates) to forecast future bed demand. This allows hospitals to proactively adjust bed allocation, minimizing overcrowding and ensuring timely admissions.
- Intelligent Staff Scheduling: By considering factors like staff expertise, patient acuity, and predicted workload, ML algorithms can create optimized staff schedules. This minimizes staffing shortages, reduces overtime costs, and ensures appropriate staffing levels across different departments.
- Supply Chain Optimization: ML can analyze consumption patterns of medical supplies to predict future needs, reducing waste from overstocking and preventing shortages. This leads to cost savings and ensures that essential supplies are always available.
Improved Patient Flow and Reduced Wait Times
Long wait times are a common source of frustration for patients and a significant operational challenge for hospitals. Machine learning offers several ways to improve patient flow and reduce these delays.
Machine learning is revolutionizing healthcare, from diagnosing diseases earlier to personalizing treatments. This predictive power isn’t limited to medicine; it’s also boosting accuracy in other fields, like weather forecasting, as you can see in this fascinating article: How Machine Learning is Improving the Accuracy of Weather Forecasting. The ability to analyze massive datasets and identify subtle patterns benefits both areas, ultimately leading to better outcomes for patients and more reliable predictions for everyone.
For instance, ML-powered appointment scheduling systems can optimize appointment slots based on patient needs and provider availability, minimizing scheduling conflicts and reducing patient wait times. Similarly, predictive models can anticipate potential bottlenecks in the emergency department or other high-traffic areas, allowing hospitals to proactively adjust staffing and resources to manage patient flow more efficiently. Imagine a system that can accurately predict surge times in the ER based on weather patterns, local events, or even social media trends – a powerful tool for proactive resource management.
Predictive Maintenance of Medical Equipment
Medical equipment downtime is costly and can disrupt patient care. Machine learning can significantly improve the reliability of medical equipment through predictive maintenance.
By analyzing sensor data from medical devices, ML algorithms can identify patterns that indicate potential equipment failures. This allows for proactive maintenance, preventing unexpected breakdowns and minimizing costly downtime. For example, an ML model might predict the imminent failure of an MRI machine based on subtle changes in its operating parameters, allowing for scheduled maintenance before the machine fails and disrupts patient appointments. This not only saves money but also ensures the continued availability of critical medical equipment.
Addressing Healthcare Disparities
Source: authorea.com
Machine learning holds immense potential to revolutionize healthcare, but its impact must be equitable. The current healthcare system often reflects existing societal biases, leading to disparities in access, quality, and outcomes for different demographic groups. However, by carefully designing and deploying machine learning algorithms, we can actively work towards a more just and inclusive healthcare landscape. This involves not only identifying and mitigating biases within the data and algorithms themselves but also leveraging the technology to improve access to care for underserved populations.
Machine learning can help identify and mitigate biases in healthcare data and algorithms by employing techniques designed to detect and correct for unfairness. This involves scrutinizing datasets for imbalances in representation across different demographic groups and developing algorithms that are less susceptible to perpetuating these biases. For instance, algorithms trained on data predominantly from one demographic group might perform poorly or even exhibit discriminatory behavior when applied to other groups. Techniques like fairness-aware machine learning, which incorporates fairness constraints into the model training process, are crucial in addressing this challenge. Regular audits and independent verification of algorithms are also necessary to ensure ongoing fairness and prevent unintended bias from creeping in.
Bias Mitigation Strategies in Machine Learning for Healthcare
Addressing bias requires a multi-pronged approach. First, data collection must be more inclusive, ensuring that datasets accurately reflect the diversity of the patient population. This might involve targeted data collection efforts in underserved communities and the development of data sharing agreements that protect patient privacy while promoting data accessibility for research and algorithm development. Second, algorithmic fairness techniques, such as re-weighting samples or using adversarial training, can help minimize bias during model training. Finally, ongoing monitoring and evaluation of algorithms in real-world settings are critical to identify and address any emerging biases. For example, if an algorithm consistently misdiagnoses a condition in a specific demographic group, it signals the need for further investigation and refinement. This continuous feedback loop is crucial for ensuring long-term fairness and equity.
Improving Healthcare Access in Underserved Communities, How Machine Learning Algorithms Are Improving Healthcare Outcomes
Machine learning is already being used to improve healthcare access in underserved communities in several ways. Telemedicine platforms, powered by machine learning algorithms for image analysis and remote patient monitoring, can extend the reach of healthcare providers to rural or geographically isolated areas. These platforms can help diagnose conditions, monitor patient progress, and provide timely interventions, reducing the need for costly and time-consuming travel to urban healthcare centers. Furthermore, machine learning can be used to predict which patients are most likely to experience health complications or require urgent care, allowing for proactive interventions and improved resource allocation. This is particularly valuable in underserved communities where access to preventative care may be limited. For instance, a machine learning model could predict which individuals in a low-income neighborhood are at high risk of developing diabetes, enabling targeted interventions like health education programs or early screening.
A Strategy for Addressing Health Disparities Related to Specific Demographics
A comprehensive strategy for using machine learning to address health disparities needs to be tailored to the specific needs of each demographic group. This involves careful consideration of the unique social, economic, and cultural factors that contribute to health disparities within these groups. For example, addressing health disparities among the elderly might involve developing machine learning algorithms to predict falls or cognitive decline, enabling timely interventions and improved quality of life. For racial and ethnic minority groups, it might involve creating culturally sensitive algorithms that account for genetic variations and health beliefs. In each case, community engagement and collaboration are crucial for ensuring that the machine learning solutions are relevant, acceptable, and effective within the target population. Successful implementation requires a strong partnership between researchers, healthcare providers, and community leaders to ensure that technology serves as a tool for health equity, rather than exacerbating existing inequalities.
Conclusive Thoughts: How Machine Learning Algorithms Are Improving Healthcare Outcomes
The integration of machine learning into healthcare is no longer a futuristic concept; it’s a present-day reality with transformative potential. While challenges remain, the benefits – from faster, more accurate diagnoses to personalized treatments and more efficient healthcare systems – are undeniable. As algorithms continue to evolve and datasets grow, the impact of machine learning on healthcare outcomes will only become more profound, promising a future where healthcare is more precise, effective, and equitable for everyone.
