The Future of Smart Healthcare Devices in Managing Chronic Diseases is here, and it’s seriously game-changing. Forget clunky, inconvenient treatments; we’re talking sleek tech that puts patients in the driver’s seat of their own health. From wearable sensors that track vital signs in real-time to AI-powered algorithms predicting potential issues, this revolution is transforming how we tackle persistent health challenges. This isn’t just about better gadgets; it’s about empowering individuals and fundamentally reshaping the healthcare landscape.
Imagine a world where chronic conditions are managed proactively, not reactively. Smart devices are paving the way for this future, offering personalized insights, early warning systems, and improved adherence to treatment plans. This means fewer hospital visits, a better quality of life, and ultimately, healthier, happier lives. But, as with any technological leap, there are hurdles to overcome, including data privacy concerns and ensuring equitable access for everyone. Let’s dive into the exciting possibilities and the challenges that lie ahead.
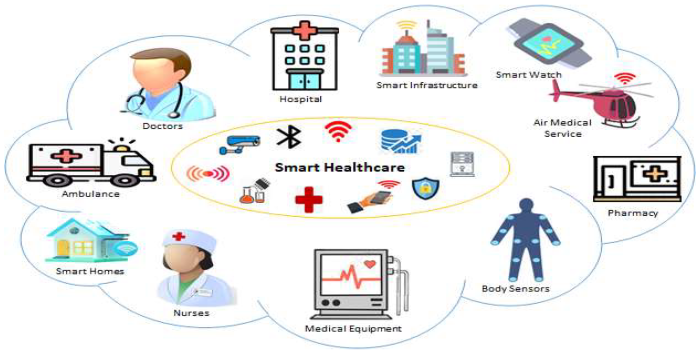
Technological Advancements in Smart Healthcare Devices
The past decade has witnessed a dramatic transformation in how we manage chronic diseases, largely driven by the rapid evolution of smart healthcare devices. These aren’t just glorified fitness trackers; they’re sophisticated tools capable of collecting, analyzing, and transmitting vital health data, empowering both patients and healthcare providers to make more informed decisions. This shift has led to improved patient outcomes, reduced hospitalizations, and a more proactive approach to disease management.
Evolution of Smart Healthcare Devices
The journey of smart healthcare devices has been marked by a significant increase in miniaturization, improved sensor accuracy, and enhanced connectivity. Early devices were bulky and limited in their functionality, often focusing solely on a single metric like heart rate. Today, we see devices that seamlessly integrate multiple sensors, providing a holistic view of a patient’s health status. This evolution has been fueled by advancements in microelectronics, wireless communication technologies, and data analytics. For example, continuous glucose monitors (CGMs) have moved from large, externally worn devices to smaller, less intrusive sensors that can be worn for extended periods. Similarly, insulin pumps have become more sophisticated, incorporating features like automated insulin delivery based on CGM data.
Key Technological Breakthroughs
Three key technological breakthroughs have revolutionized the efficacy of smart healthcare devices in chronic disease management:
1. Miniaturization and improved sensor technology: Smaller, more accurate sensors allow for continuous and unobtrusive monitoring of vital signs, leading to earlier detection of potential health issues. Think of the evolution of wearable ECG monitors, moving from bulky chest straps to small, wrist-worn devices capable of detecting arrhythmias with remarkable accuracy.
2. Advanced wireless communication and data transfer: Seamless integration with smartphones and cloud-based platforms enables real-time data sharing between patients, doctors, and caregivers. This facilitates remote monitoring and timely interventions, crucial for managing conditions like heart failure or diabetes where rapid responses can be life-saving. For instance, a patient with atrial fibrillation can have their ECG data transmitted directly to their cardiologist, allowing for immediate assessment and treatment.
3. Improved battery life and power management: Longer battery life allows for extended periods of continuous monitoring without the need for frequent charging, enhancing patient compliance and data continuity. This is especially crucial for implantable devices, where battery replacement can be a significant undertaking. The development of low-power, energy-efficient components has significantly extended the lifespan of these devices.
The Role of AI and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are transforming the capabilities of smart healthcare devices. AI algorithms can analyze vast amounts of patient data to identify patterns, predict potential health risks, and personalize treatment plans. ML models, for instance, can be trained to recognize subtle changes in heart rate variability that might indicate an impending cardiac event, allowing for proactive intervention. This predictive capability is invaluable in managing chronic conditions, allowing for preventative measures rather than reactive treatments. Moreover, AI can assist in automating tasks like insulin delivery optimization in diabetes management or personalized medication reminders for adherence.
Wearable Sensors vs. Implantable Devices
Wearable sensors and implantable devices both play critical roles in chronic disease monitoring, but they differ significantly in their functionalities and applications. Wearable sensors, such as smartwatches and fitness trackers, offer convenience and ease of use, but their data may be less accurate and prone to interference from external factors. Implantable devices, such as pacemakers and neurostimulators, provide more precise and continuous data but require invasive procedures for implantation and carry associated risks. The choice between wearable and implantable devices depends on the specific chronic condition, the desired level of monitoring accuracy, and the patient’s individual circumstances.
Comparison of Smart Healthcare Devices
| Device Type | Chronic Disease | Application | Key Features |
|---|---|---|---|
| Continuous Glucose Monitor (CGM) | Diabetes | Continuous glucose monitoring, insulin dose adjustments | Real-time glucose readings, alerts for high/low glucose |
| Insulin Pump | Diabetes | Automated insulin delivery | Programmable insulin delivery, integration with CGM |
| Smart Inhaler | Asthma, COPD | Medication tracking, adherence monitoring | Records inhalation times, dosage, and frequency |
| Wearable ECG Monitor | Heart disease | Continuous heart rhythm monitoring, arrhythmia detection | Real-time ECG readings, alerts for irregular heartbeats |
Impact on Patient Outcomes and Quality of Life
Smart healthcare devices are revolutionizing chronic disease management, significantly impacting patient outcomes and overall quality of life. These devices, ranging from wearable fitness trackers to implantable sensors, are not just technological marvels; they’re powerful tools empowering patients and transforming how healthcare is delivered. The shift is moving away from reactive, episodic care towards proactive, personalized management, leading to better health and improved well-being.
Improved Patient Adherence to Treatment Plans
Smart devices are proving remarkably effective in improving patient adherence to treatment plans. For example, medication reminders sent directly to a patient’s smartphone can significantly reduce missed doses, a common problem for individuals managing chronic conditions like diabetes or hypertension. Furthermore, features like activity trackers encourage patients to engage in regular exercise, a crucial component of many chronic disease management plans. Data collected by these devices provides valuable insights into patient behavior, allowing healthcare providers to identify potential adherence issues early and intervene proactively. This personalized approach, tailored to individual needs and preferences, increases the likelihood of successful treatment outcomes.
Patient Empowerment in Health Management
Smart healthcare devices are empowering patients to take control of their health. Instead of passively receiving treatment, individuals can actively monitor their vital signs, track their progress, and make informed decisions based on real-time data. This enhanced self-management capability fosters a sense of responsibility and ownership, leading to greater engagement and improved outcomes. For instance, a diabetic patient using a continuous glucose monitor can adjust their insulin dosage based on immediate blood sugar readings, preventing dangerous fluctuations. This level of control and personalized feedback empowers patients to actively participate in their care, transforming them from passive recipients into active partners in their healthcare journey.
Real-time Data and Early Intervention
The ability of smart devices to collect and transmit real-time data is a game-changer for early detection and intervention in chronic disease progression. For example, a smartwatch detecting an irregular heartbeat can alert the patient and their physician, potentially preventing a serious cardiac event. Similarly, continuous glucose monitors can detect early signs of hypoglycemia or hyperglycemia, allowing for timely intervention and preventing complications. This proactive approach, facilitated by the constant monitoring and data analysis capabilities of smart devices, drastically improves the chances of managing chronic conditions effectively and preventing serious health crises.
Case Studies: Positive Impacts on Quality of Life
Consider a patient with congestive heart failure. A smart device monitoring their heart rate and activity levels can alert them and their doctor to potential worsening of their condition, allowing for timely adjustments to medication or lifestyle changes, preventing hospitalizations and improving their overall quality of life. Another example involves a patient with asthma. A smart inhaler, coupled with a sensor that tracks usage, can help patients and doctors monitor medication adherence and adjust treatment strategies as needed, leading to better control of asthma symptoms and improved respiratory health. These examples highlight how smart devices translate into tangible improvements in daily life for individuals managing chronic diseases.
Potential Benefits and Drawbacks from the Patient’s Perspective
The use of smart healthcare devices for chronic disease management offers several potential benefits, but it’s important to acknowledge the drawbacks as well.
- Benefits: Increased convenience, improved self-management, enhanced communication with healthcare providers, proactive monitoring and early detection of health issues, improved treatment adherence, increased sense of control and empowerment, and potentially better overall health outcomes and quality of life.
- Drawbacks: Potential for data privacy concerns, cost of devices and associated services, technological challenges (e.g., device malfunction, connectivity issues), potential for alarm fatigue, and the need for digital literacy and comfort with technology.
Data Management, Security, and Privacy Concerns
Source: mdpi.com
Smart healthcare devices are poised to revolutionize chronic disease management, offering personalized insights and proactive interventions. This evolution is part of a larger shift detailed in The Future of Technology-Driven Healthcare: From Diagnostics to Treatment , which explores the broader technological advancements transforming healthcare. Ultimately, these connected devices will empower individuals to take control of their health, leading to better outcomes in managing chronic conditions.
The explosion of data generated by smart healthcare devices presents a double-edged sword. While this data holds immense potential for improving patient care and advancing medical research, it also introduces significant challenges in management, security, and privacy. Effectively navigating these challenges is crucial for realizing the full benefits of this technology while safeguarding sensitive patient information.
The sheer volume and complexity of data from wearables, implantable sensors, and remote monitoring systems pose substantial hurdles. Integrating data from diverse sources, ensuring data quality and consistency, and developing efficient analytical tools capable of extracting meaningful insights are all significant undertakings. Furthermore, the need to interpret this data in the context of individual patient characteristics and clinical history adds another layer of complexity. For example, a slightly elevated heart rate reading from a smartwatch might be inconsequential for a healthy individual, but could be a critical warning sign for someone with a pre-existing heart condition. The system must be sophisticated enough to make these crucial distinctions.
Challenges in Managing and Interpreting Large Volumes of Data
Smart healthcare devices generate massive amounts of data, encompassing physiological measurements, activity levels, environmental factors, and more. This data often comes in various formats and from disparate sources, making integration and analysis a complex task. Developing robust algorithms capable of handling noisy data, identifying patterns, and providing clinically relevant insights requires significant computational power and sophisticated data science expertise. The development of effective data visualization tools is also essential for clinicians to easily interpret the vast amount of information generated, facilitating timely and informed decision-making. For instance, a clinician needs to quickly understand the trends in a patient’s blood glucose levels over a period of weeks, not just individual readings.
Secure Data Storage and Transmission System Design
A secure data storage and transmission system for sensitive patient health information must adhere to stringent security protocols. This includes employing robust encryption techniques during both data storage and transmission, utilizing multi-factor authentication for access control, and implementing regular security audits to identify and address vulnerabilities. The system should also comply with relevant data privacy regulations such as HIPAA in the US or GDPR in Europe. A layered security approach, incorporating firewalls, intrusion detection systems, and regular software updates, is essential to minimize the risk of data breaches. Data anonymization and de-identification techniques should be employed whenever possible to further protect patient privacy. Consider a system where data is stored on encrypted servers, with access granted only to authorized healthcare professionals via secure, encrypted channels.
Ethical Implications of Using Patient Data for Research and Development
The use of patient data collected by smart healthcare devices for research and development purposes raises important ethical considerations. Informed consent is paramount. Patients must be fully informed about how their data will be used, who will have access to it, and the potential risks and benefits involved. Transparency and data governance frameworks are crucial to ensure that data is used responsibly and ethically. Researchers must also address issues of data bias and fairness, ensuring that algorithms and models developed using this data do not perpetuate existing health disparities. For example, algorithms trained primarily on data from one demographic group might not perform well for other groups, leading to inaccurate diagnoses or treatment recommendations.
Potential Privacy Risks and Mitigation Strategies
Smart healthcare devices collect highly sensitive personal information, raising concerns about potential privacy violations. Data breaches, unauthorized access, and the potential for data re-identification pose significant risks. Mitigation strategies include implementing strong data encryption, access control mechanisms, and robust privacy policies. Regular security audits and penetration testing can help identify and address vulnerabilities. Data minimization—collecting only the necessary data—and data anonymization techniques can further reduce privacy risks. Furthermore, educating patients about the potential risks and empowering them to control their data is crucial. For example, patients should be able to easily access and manage their data, and have the option to delete it if they choose.
Best Practices for Ensuring Data Security and Patient Privacy
To ensure data security and patient privacy, several best practices should be implemented:
- Implement robust encryption for both data at rest and in transit.
- Utilize strong access control mechanisms, including multi-factor authentication.
- Regularly conduct security audits and penetration testing.
- Comply with all relevant data privacy regulations (e.g., HIPAA, GDPR).
- Employ data anonymization and de-identification techniques whenever possible.
- Develop transparent and comprehensive privacy policies.
- Educate patients about data privacy and security risks.
- Provide patients with control over their data, including the ability to access, modify, and delete it.
- Implement a robust incident response plan to address data breaches effectively.
Integration with Healthcare Systems and Future Trends
The integration of smart healthcare devices into existing healthcare systems is still in its nascent stages, presenting both exciting opportunities and significant hurdles. While some devices seamlessly connect with electronic health records (EHRs), many others operate in silos, hindering the potential for comprehensive data analysis and personalized care. The future, however, promises a much more cohesive landscape, where data flows freely and intelligently between devices and healthcare providers.
The current state of integration is characterized by a patchwork of solutions. Some hospitals and clinics have successfully implemented systems that allow data from wearable devices, such as continuous glucose monitors or smartwatches, to be directly uploaded to patient EHRs. This facilitates more informed clinical decision-making. However, interoperability remains a major challenge; different devices often use incompatible data formats and communication protocols, creating barriers to seamless data exchange. Furthermore, the sheer volume of data generated by these devices requires robust and scalable data management solutions.
Remote Patient Monitoring and Telehealth Facilitation
Smart healthcare devices are revolutionizing remote patient monitoring (RPM) and telehealth services. Imagine a scenario where a patient with congestive heart failure wears a smart patch that continuously monitors their heart rate, blood pressure, and oxygen saturation. This data is transmitted wirelessly to a secure cloud platform, where it’s analyzed by algorithms that detect potential problems. If an anomaly is detected, the system automatically alerts the patient’s physician, who can then intervene promptly, potentially preventing a hospital visit. This type of proactive monitoring is particularly beneficial for patients with chronic conditions who require frequent check-ups. The use of video conferencing and remote diagnostic tools further enhances telehealth capabilities, allowing for virtual consultations and personalized treatment plans.
Challenges and Opportunities in Diverse Healthcare Settings
Integrating smart healthcare devices into diverse healthcare settings presents both unique challenges and opportunities. In resource-limited settings, the cost of devices and the need for reliable internet connectivity can be significant barriers. However, the potential benefits of improved patient outcomes and reduced healthcare costs are compelling. Moreover, the use of these devices can empower patients to take a more active role in managing their own health, leading to greater self-efficacy and improved adherence to treatment plans. Addressing issues of digital literacy and ensuring equitable access to technology are crucial to realizing the full potential of smart healthcare devices in diverse populations.
Future Trends in Smart Healthcare Device Development, The Future of Smart Healthcare Devices in Managing Chronic Diseases
Over the next 5-10 years, we can expect significant advancements in the development and application of smart healthcare devices for chronic disease management. Artificial intelligence (AI) and machine learning (ML) will play a pivotal role in analyzing data from these devices to provide more accurate diagnoses, personalized treatment recommendations, and proactive alerts. The development of more sophisticated sensors and miniaturized devices will lead to improved comfort and usability. We can also anticipate increased integration with other technologies, such as virtual reality (VR) and augmented reality (AR), to enhance patient engagement and treatment adherence. For instance, imagine VR-based rehabilitation programs for stroke patients, guided by data from wearable sensors that track their progress.
A Hypothetical Future Scenario: Seamless Integration
Imagine a future where a person diagnosed with type 2 diabetes seamlessly integrates a suite of smart healthcare devices into their daily life. A smart insulin pen automatically adjusts insulin delivery based on continuous glucose monitoring data. A smart scale monitors weight and body composition, providing feedback on dietary adherence. A smartwatch tracks physical activity levels, providing incentives for regular exercise. All this data is securely transmitted to a central platform, accessible to both the patient and their healthcare team. The system utilizes AI to identify potential complications early on, providing personalized recommendations and alerts to prevent hospitalizations. If blood sugar levels consistently remain high despite adjustments, the system automatically schedules a virtual consultation with an endocrinologist. This comprehensive system fosters proactive management, empowering the patient to actively participate in their care and significantly improving their quality of life.
Cost-Effectiveness and Accessibility: The Future Of Smart Healthcare Devices In Managing Chronic Diseases
The integration of smart healthcare devices into chronic disease management presents a compelling case for improved health outcomes, but their widespread adoption hinges on addressing cost-effectiveness and accessibility. While initial investment might seem high, a comprehensive analysis reveals potential long-term cost savings and improved quality of life, particularly when considering the escalating costs associated with traditional chronic disease management. However, disparities in access based on socioeconomic factors necessitate strategies to ensure equitable distribution and affordability.
Cost Comparison of Smart Devices Versus Traditional Methods
Traditional chronic disease management often relies on frequent doctor visits, extensive lab tests, and potentially costly medications. These methods can lead to significant expenses, especially for patients with multiple chronic conditions requiring ongoing care. Smart healthcare devices, on the other hand, offer the potential to reduce these costs through remote monitoring, early detection of complications, and personalized interventions. For example, continuous glucose monitors (CGMs) for diabetes patients can prevent severe hyper- or hypoglycemic events, reducing the need for emergency room visits and hospitalizations. Similarly, remote blood pressure monitoring can allow for timely adjustments to medication, preventing potentially costly cardiovascular events. While the upfront cost of the devices can be a barrier, the long-term cost savings from reduced hospitalizations and improved disease management can be substantial. This shift from reactive to proactive care is a key driver of cost-effectiveness.
Factors Influencing Accessibility and Affordability
Several factors influence the accessibility and affordability of smart healthcare devices. The initial purchase price of devices can be prohibitive for many individuals, particularly those with limited incomes. Furthermore, ongoing costs such as data plans, app subscriptions, and replacement parts can create a financial burden. Access to reliable internet connectivity is also crucial for effective device utilization, posing a challenge for individuals in underserved areas with limited digital infrastructure. Health literacy and technological proficiency also play significant roles; individuals who are unfamiliar with technology may find these devices difficult to use, limiting their effectiveness and potentially leading to abandonment. Finally, reimbursement policies by insurance providers significantly impact affordability. Limited coverage or high out-of-pocket expenses can restrict access to these technologies.
Strategies to Improve Accessibility for Underserved Communities
Improving accessibility for underserved communities requires a multi-pronged approach. Government subsidies and financial assistance programs can help reduce the initial cost of devices for low-income individuals. Public-private partnerships can be leveraged to provide affordable data plans and technical support. Community-based education programs can enhance health literacy and improve technological proficiency. Furthermore, insurance providers need to expand coverage for smart healthcare devices and reduce out-of-pocket expenses. Finally, the development of user-friendly interfaces and culturally appropriate educational materials can ensure that these devices are accessible and usable for diverse populations.
Cost-Benefit Analyses of Widespread Adoption
Cost-benefit analyses are crucial for evaluating the economic impact of widespread smart healthcare device adoption. These analyses compare the total costs of implementing and maintaining the devices (including purchase price, maintenance, data plans, and training) with the potential benefits, such as reduced hospitalizations, improved patient outcomes, increased productivity, and reduced healthcare utilization. For example, a study could compare the cost of managing a population of diabetic patients using traditional methods versus using CGMs and remote monitoring. By quantifying the cost savings from reduced hospital admissions and improved glycemic control, the analysis can determine the overall economic benefit of widespread CGM adoption. These analyses need to consider both direct costs (e.g., device cost, healthcare utilization) and indirect costs (e.g., lost productivity due to illness), as well as the long-term effects on healthcare spending.
Cost Comparison of Smart Healthcare Devices
| Device Type | Approximate Initial Cost (USD) | Potential Long-Term Cost Savings (USD/year, estimated) | Notes |
|---|---|---|---|
| Continuous Glucose Monitor (CGM) | 1000-3000 | 500-2000 | Savings vary based on frequency of hospitalizations and complications avoided. |
| Smart Blood Pressure Monitor | 50-200 | 100-500 | Savings primarily from reduced need for doctor visits and medication adjustments. |
| Smart Inhaler | 100-300 | 200-800 | Savings from improved medication adherence and reduced exacerbation rates. |
| Wearable Activity Tracker with Health Monitoring | 50-200 | Variable, often indirect savings through improved health and lifestyle changes. | Savings may be difficult to quantify directly but can contribute to overall cost reduction. |
Concluding Remarks
The future of chronic disease management is undeniably intertwined with the advancement of smart healthcare devices. While challenges remain in terms of data security, accessibility, and system integration, the potential benefits are immense. From empowering patients to take control of their health to enabling proactive interventions and improved quality of life, these devices are poised to revolutionize how we approach persistent health issues. The journey is ongoing, but the direction is clear: a future where technology empowers individuals to live healthier, longer lives.
