The Role of Augmented Reality in Improving Physical Therapy – Augmented Reality: Revolutionizing Physical Therapy is no longer a futuristic fantasy; it’s reshaping how we approach rehabilitation. Forget clunky equipment and monotonous exercises – AR is injecting a dose of interactive fun into physical therapy, boosting patient engagement and accelerating recovery. Imagine virtual reality-like games that help stroke patients regain motor skills or interactive apps guiding seniors through balance exercises. This isn’t just about tech; it’s about empowering patients and pushing the boundaries of traditional therapy.
This article dives deep into the ways augmented reality is transforming physical therapy, from its practical applications in treating various conditions to the technological advancements driving this exciting field. We’ll explore the benefits, challenges, and future potential of AR in creating a more engaging, effective, and personalized approach to physical rehabilitation.
Introduction to Augmented Reality (AR) in Physical Therapy
Traditional physical therapy, while effective, often faces challenges in patient engagement, adherence, and personalized treatment. Limited access to specialized therapists, difficulty in visualizing exercises, and a lack of real-time feedback contribute to these limitations. Patients may struggle to understand complex instructions, leading to incorrect form and potentially hindering recovery. This is where augmented reality (AR) steps in, offering a revolutionary approach to overcome these hurdles.
AR technology overlays computer-generated images onto the real world, creating interactive and immersive experiences. In physical therapy, this means patients can visualize exercises in 3D, receive real-time feedback on their form, and engage with gamified rehabilitation programs. This enhanced engagement and personalized feedback can lead to improved patient outcomes and increased adherence to treatment plans.
Examples of AR Applications in Healthcare
AR is already making waves in various healthcare sectors. For instance, AccuVein, an AR device, projects a near-infrared light onto the patient’s skin, highlighting veins for easier intravenous access. This reduces needle sticks and improves patient comfort. Similarly, surgical navigation systems utilize AR to overlay 3D models of patient anatomy onto the surgical field, guiding surgeons with greater precision. In the context of physical therapy, AR apps guide patients through exercises, providing visual cues and tracking their movements. One example is a system that overlays a virtual skeleton onto a patient performing squats, providing immediate feedback on posture and range of motion. Another application involves gamified rehabilitation exercises, where patients interact with virtual environments and challenges to motivate engagement and enhance compliance.
Comparison of Traditional and AR-Enhanced Physical Therapy Methods
The following table highlights the key differences between traditional and AR-enhanced physical therapy approaches:
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Traditional Physical Therapy | Therapist-led sessions with manual instruction and observation. Relies on verbal and visual cues, often with limited real-time feedback. | Personalized attention, direct therapist interaction, established efficacy for many conditions. | Can be expensive, limited access to specialized therapists, potential for inconsistent adherence, difficulty in visualizing complex movements. |
| AR-Enhanced Physical Therapy | Utilizes AR technology to provide interactive, visual, and gamified exercises with real-time feedback on form and progress. | Increased patient engagement and adherence, improved visualization of exercises, personalized feedback, potential for cost-effectiveness through remote monitoring and reduced therapist workload in some scenarios. | Requires specialized equipment and software, potential for technical glitches, initial investment costs, need for user-friendly interfaces. |
AR Applications for Specific Physical Therapy Needs
Augmented reality (AR) is revolutionizing physical therapy, offering innovative solutions for a wide range of needs. By overlaying digital information onto the real world, AR enhances patient engagement, improves exercise adherence, and provides therapists with valuable data for personalized treatment plans. This section explores specific applications of AR in physical therapy, demonstrating its potential to significantly improve patient outcomes.
AR-Enhanced Stroke Rehabilitation Exercises
AR can significantly improve rehabilitation exercises for stroke patients by making therapy more engaging and motivating. Traditional repetitive exercises can be tedious, leading to decreased patient compliance. AR applications gamify these exercises, transforming them into interactive experiences. For example, an AR application might project a virtual ball onto a table, prompting the patient to reach and grasp it, repeatedly, strengthening their affected arm. Another exercise could involve tracking the patient’s hand movements as they trace virtual shapes in the air, providing real-time feedback on range of motion and accuracy. The gamified nature of these exercises encourages patients to perform more repetitions and adhere to their therapy plans, leading to faster recovery. Further, virtual environments can simulate real-world scenarios, like reaching for objects on a shelf, providing functional training in a safe and controlled setting.
AR for Pain Management and Patient Education
AR’s ability to provide immersive and interactive experiences extends to pain management and patient education. For pain management, AR applications can guide patients through relaxation techniques, such as deep breathing exercises, visualizing calming scenes, or practicing mindfulness meditation. These techniques can be presented as interactive 3D visualizations, increasing their effectiveness and engagement. In patient education, AR can create detailed 3D models of the musculoskeletal system, allowing patients to visualize their injuries or conditions in a clear and understandable way. This improved understanding can foster better patient compliance with treatment plans and promote a sense of agency in their recovery journey. For example, an AR app could show a 3D model of a knee joint, highlighting the affected area and illustrating the therapist’s explanation of the injury and treatment plan.
AR Application for Improving Balance and Coordination in Elderly Patients
An AR application designed to improve balance and coordination in elderly patients could utilize a combination of visual and auditory cues. The application, named “BalanceBoost,” would use the device’s camera to track the patient’s movements in real-time. On-screen, the application would project a virtual pathway, perhaps a winding garden path or a balance beam, onto the patient’s surroundings. The patient would be instructed to follow the virtual pathway, maintaining their balance. The application would provide real-time feedback on their posture, sway, and step length. Auditory cues, such as gentle chimes or encouraging voice prompts, could be incorporated to provide additional guidance and motivation. Furthermore, the application could gradually increase the difficulty of the virtual pathway, challenging the patient to improve their balance and coordination progressively. The data collected by the application could be used to track the patient’s progress over time and adjust the difficulty level accordingly. This personalized approach would maximize the effectiveness of the therapy.
AR Applications for Improving Gait Analysis and Retraining
AR can revolutionize gait analysis and retraining by providing real-time, visual feedback to both the patient and the therapist. Using the device’s camera, an AR application can track a patient’s gait, overlaying digital markers on their body to highlight deviations from an ideal walking pattern. This allows therapists to identify subtle issues that might be missed during traditional observation. The application could then provide visual cues, projected onto the floor or the patient’s body, guiding them to correct their posture, stride length, and step cadence. For example, virtual arrows could indicate the direction of the foot placement, while colored lines could show the ideal trajectory of the body’s center of gravity. This real-time feedback allows for immediate corrections, accelerating the retraining process and improving the efficiency of therapy sessions. The application could also record and store gait data, allowing for progress tracking and personalized adjustments to the treatment plan.
Technological Aspects of AR in Physical Therapy

Source: healthysimulation.com
Augmented reality (AR) is revolutionizing physical therapy, offering immersive exercises and real-time feedback. This precision mirrors the advancements in robotics; think of the sophisticated automation seen in industrial settings, as detailed in this fascinating article on The Evolution of Autonomous Robots in Industrial Applications , which shows how technology enhances accuracy and efficiency. Similarly, AR in physical therapy promises more effective and personalized rehabilitation programs, ultimately leading to better patient outcomes.
Augmented reality (AR) is transforming healthcare, and physical therapy is no exception. The successful integration of AR, however, hinges on understanding the underlying technologies, their limitations, and the practical challenges of implementation within a clinical setting. This section delves into the technological aspects of AR in physical therapy, examining the various technologies used, hardware and software requirements, cost-effectiveness, and potential hurdles.
Types of AR Technologies in Physical Therapy
AR systems broadly fall into two categories: marker-based and markerless. Marker-based AR requires a visual marker, such as a printed image or a specific object, to be recognized by the AR system before it can overlay digital content. This approach offers greater accuracy and stability but limits flexibility. Markerless AR, on the other hand, utilizes the device’s camera and sensors to track the environment and overlay digital content without the need for markers. This offers increased flexibility but can be less accurate and prone to drift. In physical therapy, marker-based systems might be used for precise exercises involving specific body positions referenced to a target image, while markerless systems could be better suited for gait analysis where the patient’s movement is tracked freely in a larger space.
Hardware and Software Requirements for AR in Physical Therapy
Implementing AR in physical therapy requires specific hardware and software components. The hardware typically includes a mobile device (smartphone or tablet), a head-mounted display (HMD), or a depth camera. The choice of hardware depends on the specific application and budget. For instance, a simple application for guided exercises might only require a tablet, while a more complex system for gait analysis might require a depth camera and a powerful processing unit. Software requirements include an AR development kit (SDK), such as ARKit or ARCore, and a user interface (UI) designed for intuitive interaction. The software must also be capable of accurately tracking the patient’s movements and providing real-time feedback.
Effectiveness and Cost-Efficiency of AR Systems
The effectiveness and cost-efficiency of different AR systems vary widely depending on their complexity and features. Simpler marker-based systems using readily available tablets can be relatively inexpensive, but their functionality might be limited. More sophisticated markerless systems utilizing HMDs and advanced sensors can be significantly more expensive, requiring specialized training and maintenance. The cost-effectiveness of an AR system should be evaluated in terms of its impact on patient outcomes and the overall efficiency of the physical therapy practice. Studies are increasingly showing improved patient engagement and faster rehabilitation times with AR-assisted therapy, which can offset the initial investment. For example, a study published in the Journal of Medical Internet Research found that patients using AR-based rehabilitation exercises showed significantly better adherence compared to traditional methods.
Challenges in Implementing AR Technology in Physical Therapy Clinics
Despite its potential, several challenges hinder the widespread adoption of AR in physical therapy. The high initial cost of hardware and software can be a significant barrier for many clinics, particularly smaller ones. Furthermore, adequate training for both therapists and patients is essential to ensure proper usage and maximize the benefits of the technology. Technical issues, such as system malfunctions, connectivity problems, and software bugs, can disrupt therapy sessions and require expertise to resolve. Finally, the lack of standardized protocols and clinical guidelines for using AR in physical therapy can create uncertainty and limit its integration into routine clinical practice. Overcoming these challenges requires collaborative efforts from technology developers, healthcare professionals, and regulatory bodies.
Patient Engagement and Outcomes with AR-Assisted Therapy: The Role Of Augmented Reality In Improving Physical Therapy
Augmented reality (AR) is revolutionizing physical therapy by transforming passive exercises into interactive, engaging experiences. This shift dramatically impacts patient motivation and adherence, ultimately leading to improved recovery times and better overall outcomes. By blending the real world with digital overlays, AR fosters a more positive and effective therapeutic environment.
AR’s gamification potential is a key driver of increased patient engagement. Instead of simply following instructions, patients participate in interactive games and challenges that make rehabilitation fun and less daunting. This element of fun significantly increases adherence to prescribed exercises, a critical factor in successful physical therapy. The immersive nature of AR helps patients focus on their recovery, reducing feelings of boredom or frustration often associated with traditional therapy.
Benefits of AR-Assisted Physical Therapy for Patients
The integration of AR in physical therapy offers a range of benefits that directly contribute to improved patient outcomes. These benefits extend beyond simply making therapy more enjoyable; they translate to tangible improvements in recovery and overall well-being.
- Improved Adherence: AR’s engaging nature significantly boosts patient compliance with their prescribed exercise regimens. Gamified exercises and virtual rewards motivate patients to complete their sessions consistently.
- Faster Recovery: Increased adherence, combined with the potential for more effective and targeted exercises, often leads to faster recovery times compared to traditional methods.
- Enhanced Motivation: AR’s interactive elements and progress tracking features foster a sense of accomplishment and encourage continued participation in therapy.
- Increased Patient Satisfaction: The enjoyable and engaging nature of AR-assisted therapy often results in higher patient satisfaction levels.
- Improved Functional Outcomes: By providing real-time feedback and personalized guidance, AR can help patients achieve better functional outcomes, restoring their ability to perform everyday tasks more effectively.
Impact of AR on Patient Satisfaction and Treatment Outcomes
Studies have shown a positive correlation between the use of AR in physical therapy and improved patient satisfaction. Patients often report feeling more motivated, engaged, and empowered throughout their recovery journey. This increased engagement directly translates into better adherence to treatment plans, ultimately leading to improved functional outcomes and reduced recovery times. For example, a study published in the Journal of Medical Internet Research found that patients using AR-assisted rehabilitation for stroke recovery showed significant improvements in motor function and reported higher levels of satisfaction compared to the control group. The measurable improvements in both objective (motor function) and subjective (satisfaction) metrics highlight the transformative potential of AR.
Case Study: AR-Assisted Rehabilitation for a Rotator Cuff Injury
Imagine Sarah, a 45-year-old tennis player recovering from a rotator cuff injury. Traditional physical therapy left her feeling frustrated and demotivated. However, with AR-assisted therapy, Sarah’s experience was completely transformed. Using an AR application, she engaged in virtual tennis drills, progressively increasing the difficulty of the exercises as her strength improved. The application provided real-time feedback on her form, ensuring she performed the exercises correctly and avoiding further injury. The gamified nature of the therapy kept her motivated, and the visual feedback helped her understand her progress. As a result, Sarah adhered to her therapy plan diligently, experienced a faster recovery than anticipated, and returned to playing tennis sooner than expected, reporting significantly improved range of motion and reduced pain. This positive experience underscores the potential of AR to not only improve recovery but also to enhance the overall patient experience.
Future Trends and Research Directions in AR Physical Therapy
Augmented reality (AR) is rapidly transforming healthcare, and physical therapy is no exception. The field is poised for significant advancements, driven by ongoing research and the development of increasingly sophisticated technologies. Exploring future trends and ethical considerations is crucial to ensure responsible and effective implementation of AR in this vital area of healthcare.
Potential Future Applications of AR in Physical Therapy, The Role of Augmented Reality in Improving Physical Therapy
AR’s potential extends beyond current applications. Imagine personalized avatar-based therapy where patients interact with virtual representations of themselves, performing exercises and receiving real-time feedback on their form. Further advancements could see the integration of haptic feedback systems, providing tactile sensations that enhance the realism and effectiveness of virtual exercises. This could be particularly beneficial for patients with neurological conditions or those requiring fine motor skill rehabilitation. For example, a stroke patient might practice grasping and manipulating virtual objects, receiving immediate feedback on their grip strength and accuracy. Another area of growth is the use of AR in home-based rehabilitation programs, allowing patients to access personalized therapy remotely, under the guidance of their therapists via a connected AR system. This would dramatically increase accessibility and reduce the need for frequent clinic visits.
Current Research Trends in AR-Assisted Physical Therapy
Current research focuses on several key areas. Studies are evaluating the efficacy of AR in improving patient adherence to exercise programs, a critical factor in successful rehabilitation. Researchers are also investigating the optimal design of AR interfaces and the impact of different types of feedback (visual, auditory, haptic) on patient outcomes. A significant area of investigation involves the development of AR systems specifically tailored to address the unique needs of diverse patient populations, including those with cognitive impairments or visual limitations. For example, research is exploring the use of simplified AR interfaces and auditory cues for patients with cognitive impairments. Furthermore, research is exploring the integration of AR with other technologies, such as wearable sensors and artificial intelligence (AI), to create more personalized and adaptive therapy programs. One specific example is a study currently underway at the University of California, San Francisco, exploring the use of AI to personalize AR-based exercises based on real-time patient performance data collected through wearable sensors.
Ethical Considerations Related to Using AR in Physical Therapy
The use of AR in physical therapy raises important ethical considerations. Data privacy and security are paramount, as AR systems often collect sensitive patient data. Robust security measures are needed to protect this information from unauthorized access. Another crucial aspect is ensuring equitable access to AR-assisted therapy. The cost of AR technology and the digital literacy required to use it effectively could create disparities in access to care. Therefore, strategies to make AR therapy affordable and accessible to all patients are crucial. Furthermore, the potential for over-reliance on technology and the need for maintaining the human element in therapeutic relationships must be carefully considered. Therapists need to maintain a central role in guiding and supporting patients throughout their rehabilitation journey, even as AR technology becomes more sophisticated.
A Potential Research Study Design
A randomized controlled trial (RCT) could evaluate the effectiveness of an AR application designed for post-stroke upper limb rehabilitation. Participants would be randomly assigned to either an AR-assisted therapy group or a standard therapy group. The AR group would use a tablet-based application that guides them through a series of virtual exercises involving object manipulation and functional tasks, providing real-time feedback on their performance. The standard therapy group would receive traditional upper limb rehabilitation. Outcome measures would include range of motion, grip strength, functional ability (using standardized assessments like the Fugl-Meyer Assessment), and patient-reported outcomes (e.g., quality of life, satisfaction with therapy). Data analysis would compare the two groups to determine the effectiveness of the AR intervention. This study would rigorously evaluate the clinical efficacy and cost-effectiveness of AR-assisted therapy, providing valuable evidence to guide its implementation in clinical practice.
Concluding Remarks
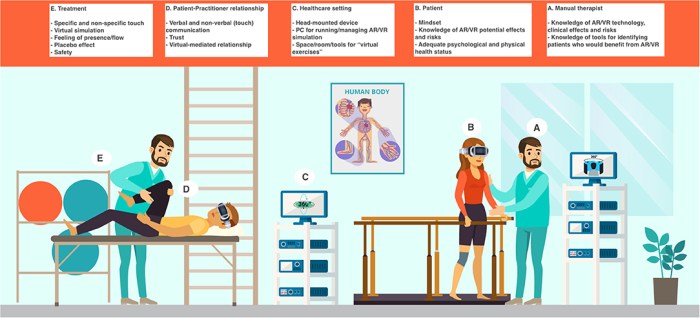
Source: frontiersin.org
The integration of augmented reality in physical therapy is not just a technological upgrade; it’s a paradigm shift. By enhancing patient engagement, personalizing treatment plans, and objectively measuring progress, AR promises a future where rehabilitation is more effective, accessible, and enjoyable. While challenges remain, the potential for AR to revolutionize physical therapy is undeniable, paving the way for faster recovery, improved patient outcomes, and a more holistic approach to healthcare.
